New york state pharmacy regulations
If you are a resident of New York State and are in need of prescription medications, it is crucial to understand the state's pharmacy regulations. These regulations are put in place to ensure the safe and effective dispensing of medications to the public. By being aware of these regulations, you can make informed decisions about your healthcare and ensure that you are receiving the best possible care.
One important aspect of the New York State pharmacy regulations is the requirement for pharmacies to be licensed by the State Board of Pharmacy. This licensing process involves a thorough review of the pharmacy's operations, including the qualifications of the pharmacists on staff and the quality of the medications being dispensed. By choosing a licensed pharmacy, you can have confidence that your medications are being handled by knowledgeable professionals.
In addition to licensing, New York State pharmacy regulations also include strict guidelines for the storage and handling of medications. These guidelines are in place to prevent contamination and ensure the integrity of the medications. Pharmacies are required to have specific storage conditions for different types of medications, such as refrigeration for certain drugs. By adhering to these regulations, pharmacies can help to ensure that medications are safe and effective for patients.
Another important aspect of the New York State pharmacy regulations is the requirement for pharmacies to maintain patient confidentiality. This means that pharmacies are not allowed to disclose any information about a patient's medications or medical conditions without the patient's consent. This protection of patient privacy is crucial in maintaining trust between healthcare providers and patients and ensuring that patients feel comfortable seeking healthcare services.
In conclusion, understanding the New York State pharmacy regulations is essential for residents in need of prescription medications. By being aware of these regulations, you can ensure that you are receiving safe and effective healthcare. Whether it is choosing a licensed pharmacy or ensuring the proper storage of medications, these regulations are in place to protect your well-being. So, take the time to familiarize yourself with the regulations and make informed decisions about your healthcare.
New York State Pharmacy Regulations: An Overview
1. Licensing and Registration Requirements
All pharmacies operating in the state of New York must be licensed and registered with the New York State Board of Pharmacy. This includes both retail and institutional pharmacies. Pharmacists and pharmacy technicians must also be licensed to practice in the state.
2. Prescription Drug Monitoring Program (PDMP)
New York State has implemented a Prescription Drug Monitoring Program to help prevent prescription drug abuse and diversion. This program requires pharmacies to report information on controlled substance prescriptions to a central database. Health care providers can access this database to review a patient's prescription history before prescribing medications.
3. Patient Counseling Requirements
Pharmacists in New York State are required to offer patient counseling services for all new prescriptions. This includes providing information on proper medication use, potential side effects, and any other relevant information. Pharmacy staff should make an effort to ensure that patients understand their medications and can safely use them.
4. Compounding Regulations
New York State has specific regulations regarding compounding, which is the process of preparing customized medications. Pharmacies that engage in compounding must comply with strict quality standards to ensure patient safety. Additionally, sterile compounding must be done in compliance with USP guidelines.
5. Controlled Substance Dispensing and Reporting
Pharmacies in New York State must comply with regulations regarding the dispensing of controlled substances. These include maintaining accurate records of dispensed medications, properly storing and securing controlled substances, and reporting any suspicious or potentially illegal activities to the appropriate authorities.
6. Electronic Prescribing
New York State has implemented regulations requiring the electronic prescribing of all medications, except in certain circumstances. This helps to reduce errors and promote efficiency in the prescribing and dispensing process. Both prescribers and pharmacies must comply with these regulations.
7. Pharmacy Inspections and Audits
The New York State Board of Pharmacy conducts regular inspections and audits of pharmacies to ensure compliance with regulations. These inspections may include a review of pharmacy practices, record keeping, medication storage, and adherence to patient counseling requirements. Pharmacies found to be in violation of regulations may be subject to penalties and fines.
8. Continuing Education Requirements
Pharmacists and pharmacy technicians in New York State are required to complete a certain number of continuing education credits to maintain their licenses. These credits must be earned through approved educational programs and are designed to ensure that professionals stay up-to-date with the latest developments in pharmacy practice.
9. Medication Error Reporting
All pharmacies in New York State are required to have a medication error reporting system in place. This allows for the identification and analysis of errors to prevent future occurrences and improve patient safety. The reporting of medication errors is confidential and protected from legal discovery.
10. Board of Pharmacy Oversight
The New York State Board of Pharmacy is responsible for overseeing and enforcing pharmacy regulations in the state. The board is composed of pharmacists and public members appointed by the governor. Their role is to protect the public's health and safety by ensuring pharmacies and pharmacy professionals adhere to the highest standards of practice.
Licensing Requirements for Pharmacists
Educational Requirements:
In order to become licensed as a pharmacist in the state of New York, individuals must first complete a Doctor of Pharmacy (PharmD) degree from an accredited pharmacy program. This includes a rigorous curriculum that covers topics such as pharmacology, pharmaceutical calculations, drug interactions, and patient counseling.
Examination:
After completing their educational requirements, aspiring pharmacists must pass the North American Pharmacist Licensure Examination (NAPLEX). This is a comprehensive exam that assesses a candidate's knowledge and skills in pharmacy practice. In addition, candidates must also pass the Multistate Pharmacy Jurisprudence Examination (MPJE), which tests their knowledge of the laws and regulations governing pharmacy practice in New York State.
Experience:
Along with their educational and examination requirements, candidates for pharmacist licensure in New York must also complete a designated period of supervised practical experience. This typically involves working under the supervision of a licensed pharmacist in a pharmacy setting, such as a hospital or community pharmacy. The exact number of hours required may vary, but it is generally around 1,500 hours.
Continuing Education:
Once licensed, pharmacists in New York State are required to complete continuing education courses to maintain their licensure. This helps to ensure that pharmacists stay up-to-date with the latest advancements and changes in the field of pharmacy. Pharmacists must complete a certain number of continuing education credits every three years in order to renew their license.
In summary, becoming a licensed pharmacist in the state of New York requires completion of a PharmD degree, passing the NAPLEX and MPJE exams, completing supervised practical experience, and participating in continuing education courses. These requirements are in place to ensure that pharmacists have the necessary knowledge and skills to provide safe and effective pharmaceutical care to patients in New York State.
Prescription Drug Dispensing Guidelines
1. Prescription Requirements:
In New York State, prescription drugs can only be dispensed by licensed pharmacists. To be eligible for dispensing, a prescription must be issued by an authorized prescriber, such as a physician, dentist, or nurse practitioner. The prescription must include the patient's name, the name and strength of the medication, the dosage instructions, and the prescriber's signature.
2. Prescription Labeling:
All prescription medications dispensed in New York State must be labeled properly. The label should include the patient's name, the name and strength of the medication, the dosage instructions, and the date of dispensing. Additionally, any warnings or special instructions provided by the prescriber should be clearly indicated on the label. It is the pharmacist's responsibility to ensure that the prescription label is accurate and easy to understand for the patient.
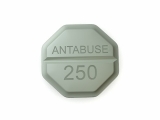
3. Controlled Substances:
There are specific guidelines for dispensing controlled substances, such as opioids, in New York State. Pharmacists must adhere to these guidelines to prevent misuse and ensure patient safety. The dispensing of controlled substances requires additional documentation, including the patient's address, the prescriber's DEA number, and the quantity of medication dispensed. Pharmacists are also required to maintain proper records of controlled substance dispensing for auditing purposes.
4. Generic Substitution:
Pharmacists in New York State are allowed to substitute generic medications for brand-name drugs, unless otherwise specified by the prescriber. This helps to reduce healthcare costs and increase access to affordable medications. However, pharmacists must ensure that the generic medication is therapeutically equivalent to the brand-name drug and that the substitution is appropriate for the patient's condition.
5. Patient Counseling:
Pharmacists have a responsibility to provide proper counseling to patients regarding their medications. This includes explaining the purpose of the medication, potential side effects, proper dosage instructions, and any precautions or warnings. Patient counseling is crucial in promoting medication adherence and preventing medication errors. Pharmacists should also encourage patients to ask questions and seek clarification if they have any concerns or doubts about their prescription.
6. Record-keeping and Documentation:
Pharmacists in New York State must maintain accurate records of medications dispensed, including patient information, prescriber details, and medication details. These records should be kept securely and should be easily accessible for auditing purposes. In addition, pharmacists should document any interactions or interventions made during the dispensing process, such as drug interactions or dosage adjustments, to ensure continuity of care and patient safety.
7. Compliance with State and Federal Laws:
Pharmacists in New York State are required to comply with state and federal laws governing the dispensing of prescription drugs. This includes ensuring the accuracy and integrity of prescription orders, preventing drug diversion and misuse, and reporting any suspected cases of fraud or abuse. Pharmacists should stay updated on the latest regulations and guidelines to maintain their professional practice and ensure the safety and well-being of their patients.
Controlled Substance Monitoring Regulations
Overview
In order to maintain the safety and security of controlled substances within pharmacies, the New York State Pharmacy Board has established strict regulations and monitoring requirements. These regulations aim to prevent the misuse, diversion, and illegal distribution of controlled substances.
Pharmacies are required to implement a comprehensive monitoring system to track the dispensing and distribution of controlled substances. This includes maintaining accurate records of all transactions, including the quantity, dosage, and patient information.
The Prescription Monitoring Program (PMP)
The New York State Prescription Monitoring Program (PMP) is a key component of the controlled substance monitoring regulations. It is an electronic database that allows pharmacists and prescribers to access information about a patient's controlled substance prescription history.
Pharmacists are required to consult the PMP before dispensing a controlled substance to ensure that the patient's prescription history is consistent with current prescribing practices and to identify any potential signs of misuse, abuse, or doctor shopping.
Reporting Requirements
Pharmacies are obligated to report certain activities related to controlled substances to the appropriate authorities. This includes suspicious orders or activities, such as unusual quantities or frequency of prescriptions, as well as any reported theft or loss of controlled substances. Failure to comply with reporting requirements can result in significant penalties and legal consequences for the pharmacy.
Additionally, pharmacies must regularly submit reports detailing their controlled substance inventory and usage to the New York State Pharmacy Board. These reports are used to monitor and evaluate pharmacies' compliance with the regulations and identify any potential issues or irregularities.
Education and Training
The New York State Pharmacy Board requires pharmacists and pharmacy staff to undergo regular education and training on controlled substance monitoring regulations. This ensures that they have a thorough understanding of their obligations and responsibilities, and are equipped with the knowledge and skills to effectively implement and comply with the regulations.
Pharmacists and staff must stay up-to-date with the latest developments in controlled substance monitoring and participate in continuing education programs to enhance their knowledge and skills. This commitment to education and training helps to maintain the integrity of the pharmacy profession and protect the public from the potential risks associated with controlled substance misuse.
Conclusion
The controlled substance monitoring regulations established by the New York State Pharmacy Board play a crucial role in ensuring the safe and responsible handling of controlled substances within pharmacies. These regulations help to prevent the misuse and illegal distribution of controlled substances, protect patients, and maintain the integrity of the pharmacy profession.
By implementing comprehensive monitoring systems, consulting the Prescription Monitoring Program, fulfilling reporting requirements, and prioritizing education and training, pharmacies can uphold their legal and ethical obligations and contribute to the overall public health and safety of the community.
Medication Error Reporting and Prevention
Medication errors can have serious consequences for patients and can lead to adverse drug reactions, hospitalizations, and even death. It is crucial for pharmacies to have systems in place to report and prevent medication errors.
Reporting: Pharmacies should have a robust reporting system in place to encourage employees to report any medication errors or near misses. This can be done through an electronic reporting system or through a designated person in the pharmacy. Reporting should be confidential and anonymous to encourage open communication and prevent fear of retribution.
Investigation: When a medication error is reported, it is important for the pharmacy to conduct a thorough investigation to identify the root cause of the error. This may involve reviewing electronic records, interviewing staff involved in the process, and analyzing the workflow in the pharmacy. It is important to involve all relevant stakeholders in the investigation process, including pharmacists, pharmacy technicians, and other healthcare professionals.
Prevention: Once the root cause of a medication error is identified, pharmacies should implement appropriate measures to prevent similar errors from occurring in the future. This may include changes to the workflow, additional training for staff, and implementing new technologies or systems to help reduce the risk of errors. It is also important for pharmacies to regularly review and update their medication error prevention strategies to stay up to date with the latest best practices.
Educational Programs: Pharmacies should also invest in educational programs to train their employees on medication safety and error prevention. This can include regular training sessions, workshops, and seminars on topics such as proper medication dispensing techniques, error recognition, and communication skills. Ongoing education and training can help increase awareness of medication errors and reinforce safe practices among pharmacy staff.
Collaboration: Collaboration with other healthcare providers and organizations is essential for medication error reporting and prevention. Pharmacies should actively participate in local and national initiatives, such as medication safety collaboratives and reporting systems, to share knowledge, experiences, and best practices. By working together, healthcare providers can make significant strides in reducing medication errors and improving patient safety.
In conclusion, medication error reporting and prevention are crucial components of pharmacy practice. Implementing robust reporting systems, conducting thorough investigations, implementing prevention measures, investing in educational programs, and collaborating with other healthcare providers can help pharmacies reduce the risk of medication errors and improve patient safety.
Pharmacy Inspections and Compliance
What are pharmacy inspections?
A pharmacy inspection is a process where a regulatory authority conducts a thorough examination of a pharmacy to ensure compliance with the state's pharmacy regulations. Inspections are typically conducted at regular intervals or in response to a complaint or incident. The purpose of these inspections is to ensure that pharmacies are meeting the standards and requirements set forth by the state to protect public health and safety.
What do inspectors look for?
During a pharmacy inspection, inspectors look for various aspects of compliance, including but not limited to:
- Adherence to proper storage and handling procedures for medications
- Proper record-keeping of prescription drugs
- Verification of the credentials and qualifications of pharmacy staff
- Verification of the pharmacy's licensing and registration
- Proper labeling and packaging of medications
- Compliance with state and federal laws related to controlled substances
Consequences of non-compliance
Non-compliance with pharmacy regulations can have serious consequences. If a pharmacy fails to meet the standards set by the state, it may face penalties, fines, or even have its license revoked. Additionally, non-compliance can lead to public health risks and compromised patient safety. Therefore, it is crucial for pharmacies to ensure they are in full compliance with all relevant regulations to avoid these negative outcomes.
How to maintain compliance
To maintain compliance with pharmacy regulations, pharmacies should establish robust policies and procedures that align with the state's requirements. These should be regularly reviewed and updated as needed. It is also important to provide ongoing training and education to pharmacy staff to keep them informed of any changes in regulations. Compliance should be a top priority for pharmacies to ensure the safety and well-being of their patients.
Conclusion
Pharmacy inspections play a crucial role in ensuring that pharmacies are operating in compliance with state regulations. By adhering to proper storage and handling procedures, maintaining accurate record-keeping, and staying up-to-date with licensing and registration requirements, pharmacies can not only pass inspections but also prioritize patient safety and maintain the trust of their customers.
Continuing Education and Professional Development
Continuing education is an essential component for pharmacists in New York State to maintain their professional competence and keep up with the latest advancements in the field. Pharmacist professionals are required to complete a certain number of continuing education credits every renewal cycle to ensure that they are up to date with the ever-evolving healthcare landscape.
Pharmacists in New York State are required to complete 45 hours of continuing education every three years. These hours must include at least 3 hours of coursework on federal and state pharmacy laws and regulations, as well as at least 2 hours on infection control every three years. Additionally, at least 2 hours of continuing education must be completed in the area of opioid and other controlled substance prescriptions and as part of combating opioid overdose using naloxone.
Pharmacists have a wide range of options for obtaining continuing education credits. They can attend live conferences and seminars, participate in online courses, engage in self-study programs, or complete relevant coursework at an accredited college or university. It is important for pharmacists to ensure that the continuing education activities they participate in are approved by the Accreditation Council for Pharmacy Education (ACPE), as only ACPE-approved courses will count towards the required continuing education credits.
In addition to continuing education, pharmacists are encouraged to engage in ongoing professional development activities to enhance their skills and knowledge. This can include participating in professional organizations, attending workshops and lectures, conducting research, or pursuing additional certifications in specialized areas of pharmacy practice.
Overall, continuing education and professional development are crucial for pharmacists in New York State to stay current in their practice and provide the best possible care to patients. By continually expanding their knowledge and skills, pharmacists can effectively contribute to improving healthcare outcomes and staying ahead in a dynamic and evolving field.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "New york state pharmacy regulations"