Best time of day to take prednisone for pmr
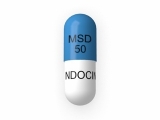
Giant cell arteritis (GCA) and polymyalgia rheumatica (PMR) are inflammatory conditions that commonly affect older individuals. PMR is characterized by widespread muscular pain and stiffness, particularly in the shoulders, upper arms, thighs, and hips. To manage the symptoms of PMR, corticosteroids like prednisone are often prescribed. Prednisone is a type of medication that suppresses inflammation and reduces swelling.
While prednisone is effective in managing the symptoms of PMR, it is essential to determine the optimal time to take it. Generally, doctors recommend taking prednisone in the morning to mimic the body's natural cortisol production. Cortisol, a hormone produced by the adrenal glands, is most abundant in the morning and gradually decreases throughout the day. By taking prednisone in the morning, it aligns with the natural cortisol rhythm and reduces the risk of interfering with sleep patterns and causing insomnia.
In addition to taking prednisone in the morning, it is crucial to follow the prescribed dosage and tapering schedule provided by the healthcare provider. Abruptly stopping prednisone can lead to adrenal insufficiency, which can have serious consequences. The tapering schedule gradually reduces the dosage over time to allow the adrenal glands to resume their normal cortisol production gradually. This approach helps minimize potential side effects and complications associated with sudden withdrawal of prednisone.
The optimal time to take prednisone for polymyalgia rheumatica (PMR)
Polymyalgia rheumatica (PMR) is a condition characterized by muscle pain and stiffness, most commonly affecting the shoulders, neck, and hips. Treatment for PMR often involves the use of prednisone, a corticosteroid medication.
When to take prednisone for PMR depends on several factors, including the severity of the symptoms and the individual's response to the medication. In general, it is recommended to take prednisone in the morning, with breakfast.
Taking prednisone in the morning helps to mimic the body's natural production of cortisol, which is highest in the morning and decreases throughout the day. By taking the medication in the morning, it can help to reduce inflammation and pain associated with PMR, and also minimize the risk of side effects.
In some cases, a healthcare provider may recommend taking prednisone in divided doses throughout the day. This can help to provide more consistent levels of the medication in the body and may be beneficial for individuals who experience symptoms later in the day.
It is important to follow the prescribed dosing instructions for prednisone and to speak with a healthcare provider about any concerns or questions regarding the optimal time to take the medication. Additionally, regular monitoring and adjustments to the dosage may be necessary to ensure the most effective treatment for PMR.
Understanding polymyalgia rheumatica (PMR)
What is polymyalgia rheumatica?
Polymyalgia rheumatica (PMR) is a common inflammatory disorder that predominantly affects older individuals. It is characterized by severe pain and stiffness in the muscles, specifically in the shoulders, neck, and hips. PMR usually occurs in people over the age of 50, and it is more common in women than in men.
Symptoms of PMR
The main symptom of PMR is muscle pain and stiffness, which are often worse in the morning or after periods of inactivity. The pain and stiffness can be debilitating and can interfere with daily activities. Other symptoms may include fatigue, weight loss, low-grade fever, and depression.
Diagnosing PMR
Diagnosing PMR can be challenging because the symptoms can be similar to those of other conditions, such as rheumatoid arthritis and fibromyalgia. However, there are specific criteria that doctors use to make a diagnosis. These criteria include the age of the individual, the duration of symptoms, the presence of morning stiffness, and the results of blood tests.
Treatment options for PMR
The mainstay of treatment for PMR is corticosteroids, such as prednisone. These medications help to reduce inflammation and relieve pain and stiffness. The dosage and duration of treatment will vary depending on the individual and their response to the medication. In some cases, other medications may be prescribed to help manage the symptoms and reduce the need for long-term corticosteroid use.
It is important for individuals with PMR to work closely with their healthcare provider to develop a treatment plan that is tailored to their specific needs and to monitor for any potential side effects of the medications.
Effectiveness of prednisone in managing PMR
Polymyalgia rheumatica (PMR) is an inflammatory condition that primarily affects older adults, causing muscle pain and stiffness in the shoulders and hips. The mainstay of treatment for PMR is prednisone, a corticosteroid drug that helps to reduce inflammation and relieve symptoms.
Prednisone has proven to be highly effective in managing PMR. It works by suppressing the immune system and reducing the production of inflammatory substances in the body. This helps to alleviate pain, stiffness, and swelling in the affected muscles.
One of the reasons prednisone is so effective in managing PMR is its rapid onset of action. Patients typically experience significant improvement in symptoms within a few days of starting treatment. This is especially important for individuals who are experiencing severe pain and difficulty with daily activities.
Another key benefit of prednisone in managing PMR is its ability to maintain long-term remission. While some patients may need to take prednisone for several months or even years, others are able to gradually reduce their dosage and eventually discontinue the medication altogether. This is a positive outcome, as long-term use of prednisone can be associated with certain side effects, such as weight gain, osteoporosis, and increased susceptibility to infections.
The dosage of prednisone for PMR varies depending on the individual and the severity of their symptoms. Typically, patients start with a higher dose and taper down to a lower maintenance dose once their symptoms are well-controlled. Regular monitoring and adjustments of the dosage may be necessary to ensure optimal symptom relief while minimizing side effects.
It is important for patients with PMR to closely follow their healthcare provider's instructions regarding prednisone usage, as sudden discontinuation or inappropriate dosage adjustments can lead to disease flares and recurrence of symptoms. Regular follow-up visits and open communication with the healthcare team are crucial for managing this condition effectively.
In conclusion, prednisone is a highly effective medication for managing PMR. It helps to reduce inflammation, alleviate symptoms, and maintain long-term remission. However, close monitoring and proper dosage adjustments are necessary to maximize its benefits and minimize potential side effects. By working closely with their healthcare providers, patients with PMR can find relief and improve their quality of life.
Factors affecting the optimal timing of prednisone intake
1. Disease-specific factors
Prednisone, a corticosteroid medication, is commonly used to manage inflammatory conditions such as polymyalgia rheumatica (PMR). The optimal timing of prednisone intake depends on various disease-specific factors.
Disease severity: The severity of PMR symptoms can vary among individuals. For some, symptoms may be more pronounced in the morning, while others may experience symptoms throughout the day. Adjusting the timing of prednisone intake based on the severity and timing of symptoms can help provide optimal relief.
Onset and duration of symptoms: PMR symptoms typically develop gradually and become worse over time. Understanding the pattern of symptom onset and duration can help determine the best time to take prednisone for maximum effect.
2. Individual patient factors
Every patient is unique, and individual factors can influence the optimal timing of prednisone intake.
Circadian rhythm: The body's natural circadian rhythm can affect drug metabolism and response. Some individuals may find that taking prednisone in the morning aligns better with their circadian rhythm, leading to improved symptom control.
Lifestyle and daily routine: Patients may have personal commitments or daily routines that affect their ability to adhere to specific medication schedules. It is important to consider these factors when determining the best time to take prednisone for each patient.
3. Medication-related factors
Certain medication-related factors can also impact the optimal timing of prednisone intake.
Pharmacokinetics: Prednisone has a relatively short half-life, meaning it is quickly metabolized and eliminated from the body. Taking prednisone at peak symptom times can ensure that therapeutic levels are maintained throughout the day.
Drug-drug interactions: Prednisone may interact with other medications, potentially affecting its absorption, distribution, or metabolism. Patients should consult with their healthcare provider to determine if there are any specific interactions that could impact the timing of prednisone intake.
Considering these factors can help healthcare providers optimize the timing of prednisone intake for each patient, ensuring maximum therapeutic benefit in the management of conditions like PMR.
The importance of morning administration
Timing is crucial when it comes to taking prednisone for polymyalgia rheumatica (PMR). It is recommended to take the medication in the morning to align with the body's natural cortisol production. Cortisol is a hormone that helps regulate inflammation and plays a vital role in managing PMR symptoms.
Beneficial effect on pain and stiffness: By taking prednisone in the morning, patients can benefit from its anti-inflammatory properties throughout the day when PMR symptoms are typically more severe. This can help alleviate pain and stiffness, making daily activities more manageable.
Minimizing side effects: Prednisone can also have side effects, such as insomnia and increased appetite. Taking the medication in the morning allows the body to have more time to process and metabolize prednisone during the day. This can help reduce the likelihood and severity of these side effects.
Enhancing patient adherence: Establishing a morning routine for taking prednisone can improve patient adherence to the medication. By associating the routine with other daily activities, such as breakfast or brushing teeth, it becomes easier for patients to remember and integrate prednisone into their daily lives.
Consult your doctor: While morning administration is generally recommended for prednisone, it is essential to follow your doctor's specific instructions. They may tailor the dosage and timing based on your individual needs and factors such as disease severity and other medications you are taking. Always consult with your healthcare provider before making any changes to your medication regimen.
Considerations for long-term prednisone use
1. Monitoring for side effects
When taking prednisone on a long-term basis, it is important to be aware of and monitor for potential side effects. Some common side effects of long-term prednisone use include weight gain, fluid retention, high blood pressure, osteoporosis, and increased risk of infections. Regular check-ups with a healthcare provider are recommended to monitor these possible side effects and adjust treatment if necessary.
2. Managing bone health
Long-term prednisone use can lead to a decrease in bone density and an increased risk of fractures. To help maintain bone health, it is important to ensure an adequate intake of calcium and vitamin D, which are essential for strong bones. In some cases, a healthcare provider may recommend a bone density test and prescribe medications such as bisphosphonates to help prevent bone loss.
3. Adrenal function
Prolonged use of prednisone can suppress the body's natural production of cortisol, which is important for regulating various bodily functions. It is essential to follow the prescribed dosage and gradually taper off the medication under the guidance of a healthcare provider to give the adrenal glands time to regain normal function. Abruptly stopping prednisone after long-term use can lead to adrenal insufficiency, characterized by fatigue, muscle weakness, and low blood pressure.
4. Eye health
Prednisone use, especially at high doses or for a prolonged period, can increase the risk of developing cataracts or glaucoma. Regular eye exams are recommended to monitor for any changes in vision or eye health. If any issues are detected, a healthcare provider may suggest appropriate interventions or adjust the prednisone dosage.
In conclusion, long-term use of prednisone requires careful monitoring and management to minimize side effects and maintain overall health. It is important to work closely with a healthcare provider to weigh the benefits and risks of prednisone use and to develop an individualized treatment plan.
Consulting with a healthcare professional for personalized prednisone dosing
Why consulting with a healthcare professional is important
When it comes to prednisone dosing for polymyalgia rheumatica (PMR), it is vital to consult with a healthcare professional. Prednisone is a powerful medication with potential side effects, and the optimal dosing regimen can vary depending on individual factors. A healthcare professional, such as a rheumatologist or primary care physician, can provide personalized guidance based on a thorough evaluation of your specific situation.
Determining the optimal prednisone dosage
During a consultation, a healthcare professional will consider several factors to determine the optimal prednisone dosage for your PMR. These factors may include the severity of symptoms, your overall health, any other medications you are taking, and any underlying medical conditions. By assessing these factors, the healthcare professional can tailor the dosage to address your specific needs while minimizing the risks of side effects.
Monitoring and adjusting the prednisone dosage
Once the prednisone dosage has been determined, it is important to regularly monitor its effectiveness and any potential side effects. Your healthcare professional will schedule follow-up appointments to evaluate your response to treatment and make any necessary adjustments to the dosage. This ongoing monitoring is essential to ensure that the prednisone is effectively managing your PMR symptoms while minimizing the risk of long-term side effects.
Educating yourself about prednisone
In addition to consulting with a healthcare professional, it is important to educate yourself about prednisone and its potential effects on your body. This can help you understand the reasons behind the recommended dosage and be aware of any warning signs or symptoms that may require immediate medical attention. Your healthcare professional can provide resources and information to help you navigate the use of prednisone and make informed decisions about your treatment.
In conclusion, consulting with a healthcare professional is crucial for personalized prednisone dosing for PMR. By working closely with a qualified provider, you can ensure that your prednisone dosage is tailored to your specific needs, monitor its effectiveness, and stay informed about potential side effects. Together, you and your healthcare professional can develop a treatment plan that is optimized for your individual circumstances and supports your overall health and well-being.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Best time of day to take prednisone for pmr"