Can people with afib take prednisone
Atrial fibrillation (Afib) is a common heart condition characterized by an irregular and often rapid heart rate. It affects millions of individuals worldwide, and managing the condition often requires a combination of medication and lifestyle changes. One medication that is commonly prescribed for various conditions, including inflammation and autoimmune disorders, is prednisone. However, many people with Afib wonder if it is safe to take prednisone, given their underlying heart condition.
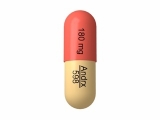
Prednisone belongs to a class of drugs called corticosteroids, which are known for their anti-inflammatory properties. They work by suppressing the immune system and reducing inflammation in the body. While prednisone can be highly effective in treating certain conditions, its use in individuals with Afib may present some risks.
One concern with prednisone use in individuals with Afib is its potential to cause or worsen fluid retention, a common symptom of heart failure. Prednisone can cause the body to retain sodium and water, leading to fluid accumulation in the tissues. This can put additional strain on the heart and exacerbate symptoms of Afib, such as shortness of breath and swelling in the legs.
Furthermore, prednisone can also increase blood pressure, which can be problematic for individuals with Afib. High blood pressure is a risk factor for heart disease and can increase the likelihood of developing complications associated with Afib, such as stroke and heart failure. Therefore, individuals with Afib who require treatment with prednisone should be closely monitored to ensure their blood pressure is well-controlled.
Understanding Atrial Fibrillation (Afib)
What is Atrial Fibrillation?
Atrial fibrillation, also known as Afib, is a heart condition characterized by irregular and rapid heartbeats. It occurs when the electrical signals that regulate heart rhythm become chaotic, causing the upper chambers of the heart (atria) to quiver or fibrillate instead of contracting properly.
Symptoms of Afib
People with Afib may experience symptoms such as palpitations, shortness of breath, fatigue, dizziness, chest pain, and fainting. However, some individuals with Afib may not have any noticeable symptoms and the condition is only discovered during routine medical check-ups.
Causes of Afib
Atrial fibrillation can be caused by various factors, including high blood pressure, heart valve problems, coronary artery disease, congenital heart defects, thyroid issues, lung diseases, excessive alcohol consumption, and stimulant drug use. In some cases, the exact cause of Afib may be unknown.
Treatment Options
Treatment for Afib aims to control the heart rate and restore normal heart rhythm. It may involve medications to regulate heart rhythm, blood thinners to reduce the risk of blood clots, lifestyle changes, and procedures such as cardioversion or catheter ablation.
In some cases, individuals with Afib may also need to manage other underlying health conditions, such as high blood pressure or diabetes, to reduce their risk of complications.
Prevention and Lifestyle Modifications
Preventing and managing Afib often involves adopting a healthy lifestyle. This may include maintaining a healthy weight, exercising regularly, avoiding excessive alcohol consumption and smoking, managing stress, and following a heart-healthy diet low in saturated fats, cholesterol, and salt.
Regular check-ups with a healthcare provider are important for individuals with Afib to monitor their condition and make necessary adjustments to their treatment plan.
What is Atrial Fibrillation?
Atrial Fibrillation (AFib) is a heart condition characterized by irregular and rapid heartbeats. It occurs when the electrical signals in the atria, the upper chambers of the heart, are chaotic and disorganized. This leads to the atria quivering instead of contracting normally, which can affect the overall efficiency of the heart's pumping action.
Symptoms of AFib include:
- Heart palpitations
- Shortness of breath
- Fatigue
- Dizziness or lightheadedness
- Chest pain or discomfort
AFib can be classified into different types, including paroxysmal AFib (intermittent episodes that last for less than 7 days), persistent AFib (continuous episodes that last for more than 7 days), and permanent AFib (continuous episodes that are ongoing and cannot be corrected).
Causes of AFib:
There can be various causes or risk factors that contribute to the development of AFib. These include:
- High blood pressure
- Heart disease
- Age (more common in people over 60)
- Obesity
- Thyroid problems
- Family history of AFib
- Excessive alcohol consumption
In some cases, the cause of AFib may be unknown.
Treatment of AFib:
Treatment for AFib aims to manage symptoms, prevent complications, and reduce the risk of stroke. The specific treatment plan may vary depending on the severity and underlying causes of AFib.
Treatment options may include:
- Medications to control heart rate and rhythm
- Blood thinners to reduce the risk of blood clots
- Cardioversion to restore normal heart rhythm
- Ablation therapy to destroy abnormal heart tissue
- Implantable devices to regulate heart rhythm
It is important for individuals with AFib to work closely with their healthcare provider to develop a personalized treatment plan that addresses their specific needs and minimizes the risk of complications.
Symptoms and Complications of Afib
Symptoms
Atrial fibrillation (Afib) is a heart condition that can lead to various symptoms. Some common symptoms include:
- Irregular heartbeat
- Rapid or fluttering heartbeat
- Heart palpitations
- Shortness of breath
- Fatigue or weakness
- Dizziness or lightheadedness
- Chest pain or discomfort
It's important to note that not everyone with Afib will experience symptoms. Some individuals may be completely asymptomatic and only discover their condition during a routine medical examination.
Complications
While Afib itself may not be life-threatening, it can lead to various complications if left untreated or poorly managed. Some complications associated with Afib include:
- Stroke: Afib increases the risk of blood clots forming in the heart, which can then travel to the brain and cause a stroke.
- Heart failure: The irregular heartbeat of Afib can weaken the heart over time, eventually leading to heart failure.
- Cardiomyopathy: Prolonged Afib can result in the enlargement or thickening of the heart muscles, a condition known as cardiomyopathy.
- Other heart conditions: Afib can also contribute to the development of other heart-related issues, such as coronary artery disease or heart attack.
Proper management of Afib, including medication, lifestyle changes, and potentially medical procedures, can help reduce the risk of complications and improve overall heart health.
Treatment Options for Atrial Fibrillation
1. Medications
Medications are often the first line of treatment for atrial fibrillation (AFib). There are several types of medications that may be prescribed to help manage the condition and control heart rhythm. These include:
- Antiarrhythmic medications: These medications help to control the heart's rhythm and prevent episodes of AFib.
- Beta blockers: Beta blockers work by slowing down the heart rate and reducing the force of contractions.
- Calcium channel blockers: This type of medication helps to relax and widen the blood vessels, improving blood flow and reducing the risk of blood clots.
- Anticoagulants: Anticoagulant medications, also known as blood thinners, are used to reduce the risk of blood clots and stroke in people with AFib.
2. Cardioversion
Cardioversion is a procedure that uses electrical shocks or medications to restore a normal heart rhythm for those with persistent or chronic AFib. This procedure can be done either through external electrodes placed on the chest or internally through a catheter.
3. Ablation
Ablation is a treatment option that aims to disrupt abnormal electrical signals in the heart that are causing AFib. During this procedure, a catheter is guided to the heart and delivers energy to destroy or scar the tissue responsible for the irregular heart rhythm.
4. Surgical Maze Procedure
The surgical maze procedure is a surgical treatment option that involves creating scar tissue in a specific pattern within the heart to disrupt the abnormal electrical signals and restore a normal heart rhythm. This procedure is typically done in conjunction with other heart surgeries, such as bypass surgery or valve repair.
5. Lifestyle Changes
In addition to medical interventions, making certain lifestyle changes can also help manage AFib. Some common lifestyle changes include:
- Quitting smoking: Smoking has been linked to an increased risk of atrial fibrillation, so quitting smoking can help reduce the frequency and severity of AFib episodes.
- Managing stress: Stress can trigger AFib episodes, so finding healthy ways to manage stress, such as through exercise, relaxation techniques, or therapy, can be beneficial.
- Eating a heart-healthy diet: A diet rich in fruits, vegetables, whole grains, lean proteins, and low in saturated fats, cholesterol, and sodium can help improve heart health and reduce the risk of AFib.
- Exercising regularly: Regular exercise can help improve cardiovascular fitness and reduce the risk of AFib. However, it's important to consult with a healthcare professional before starting a new exercise routine.
Overall, there are several treatment options available for atrial fibrillation, including medications, procedures, and lifestyle changes. It's important for individuals with AFib to work closely with their healthcare team to find the best treatment plan for their specific needs and to manage the condition effectively.
Prednisone: Uses, Side Effects, and Interactions
Uses
Prednisone is a corticosteroid medication that is commonly used to treat a variety of conditions. It works by reducing inflammation and suppressing the immune system. Prednisone is often prescribed to manage conditions such as asthma, allergies, arthritis, and certain skin disorders. It may also be used to treat certain types of cancer, as well as to prevent organ rejection after transplantation.
Side Effects
While prednisone can be effective in treating many conditions, it can also cause a range of side effects. Common side effects include increased appetite, weight gain, fluid retention, insomnia, mood changes, and increased sweating. Long-term use of prednisone can lead to more serious side effects, such as osteoporosis, high blood pressure, cataracts, and increased risk of infections.
It is important to note that the potential benefits of prednisone should be weighed against the potential risks and side effects. Your healthcare provider will consider your specific condition and medical history before prescribing this medication.
Interactions
Prednisone can interact with other medications and substances, so it is important to inform your healthcare provider about all the medications you are taking. Some medications that may interact with prednisone include certain antibiotics, antifungal medications, HIV medications, and nonsteroidal anti-inflammatory drugs (NSAIDs).
Additionally, prednisone can interact with certain vaccines, so it is important to discuss your vaccination history with your healthcare provider. It may be necessary to delay or avoid certain vaccines while taking prednisone.
Alcohol and prednisone should also be avoided, as alcohol can increase the risk of stomach ulcers and gastrointestinal bleeding.
It is important to follow your healthcare provider's instructions when taking prednisone and to report any potential interactions or side effects.
Consult Your Doctor for Personalized Advice
If you have atrial fibrillation (Afib) and are considering taking prednisone, it is important to consult with your doctor for personalized advice. While prednisone may be prescribed for certain conditions, its safety for individuals with Afib can vary depending on various factors such as the severity of your Afib, any underlying heart conditions, and other medications you may be taking.
Your doctor will be able to assess your specific medical history and provide guidance on whether or not prednisone is safe and appropriate for you. They may consider alternative medications or adjust your dosage to minimize any potential risks or interactions.
Being open and honest with your doctor about your medical history, current medications, and any concerns you may have will help them make the best decision for your individual situation. Remember that your doctor is the best person to provide personalized advice based on your unique circumstances.
It is important to note that this information is not intended to replace medical advice from a healthcare professional. Every person's medical situation is different, and what works for one individual may not be suitable for another. Therefore, it is crucial to consult with your doctor before making any decisions regarding your medication regimen, including the use of prednisone.
By working closely with your doctor, you can ensure that you are receiving the most appropriate and effective treatment for your atrial fibrillation while minimizing the potential risks associated with medication. Together, you can make informed decisions about your health and well-being.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Can people with afib take prednisone"