Can prednisone cause a skin rash
Prednisone is a commonly prescribed medication that belongs to a class of drugs called corticosteroids. It is used to treat a wide range of conditions such as allergies, asthma, autoimmune disorders, and certain types of cancer. One of the potential side effects of prednisone is skin rashes.
Skin rashes can occur as a reaction to prednisone or as a result of the underlying condition being treated. Prednisone works by suppressing the immune system, which can lead to alterations in the skin's normal functioning. This can cause various skin-related issues, including rashes, itching, and irritation.
The severity and type of skin rash can vary from person to person, and it is important to consult with a healthcare provider if you experience any changes in your skin while taking prednisone. In some cases, the rash may be mild and resolve on its own, while in others it may require additional treatment.
It is also important to note that prednisone should never be stopped abruptly without medical supervision, as this can lead to withdrawal symptoms and potential flare-ups of the underlying condition. Your healthcare provider will be able to provide guidance on the best course of action if you experience skin rashes or any other side effects while taking prednisone.
What is Prednisone?
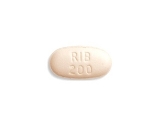
Prednisone is a medication, specifically a corticosteroid, that is used to treat various medical conditions. It is commonly prescribed to reduce inflammation in the body and suppress the immune system. Prednisone is available in different forms, including tablets, oral solution, and injections. It is classified as a prescription drug and is typically taken under the supervision of a healthcare professional.
How does Prednisone work?
Prednisone works by mimicking the actions of naturally occurring substances in the body, such as cortisol. Cortisol is a hormone produced by the adrenal glands that helps regulate inflammation and immune responses. By binding to specific receptors in the body, prednisone can block the release of certain chemicals that contribute to inflammation and suppress the activity of the immune system.
What conditions can Prednisone be used for?
- Autoimmune diseases: Prednisone is often prescribed to treat autoimmune conditions such as rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis. It helps to reduce inflammation and manage symptoms.
- Allergic reactions: Prednisone can be used to treat severe allergic reactions, including allergic rhinitis, asthma exacerbations, and contact dermatitis.
- Skin conditions: Prednisone may be prescribed for various skin conditions, such as eczema, psoriasis, and dermatitis. It can help reduce inflammation and relieve itching.
- Respiratory conditions: Prednisone may be used to treat respiratory conditions like chronic obstructive pulmonary disease (COPD) and asthma. It helps to reduce airway inflammation and improve breathing.
- Cancer: Prednisone is sometimes used as part of cancer treatment to manage symptoms such as pain, inflammation, and side effects of chemotherapy.
What are the potential side effects of Prednisone?
While prednisone can be beneficial for treating certain conditions, it can also cause various side effects. Some common side effects include increased appetite, weight gain, fluid retention, mood changes, difficulty sleeping, and increased risk of infection. Prolonged use or high doses of prednisone can also lead to more serious side effects such as osteoporosis, diabetes, and adrenal gland suppression. It is important to take prednisone as directed by a healthcare professional and to discuss any concerns or potential side effects with them.
The Link Between Prednisone and Skin Rashes
Prednisone, a corticosteroid medication, is commonly used to treat a variety of conditions, including skin rashes. While it can be an effective treatment option, it is important to understand the relationship between prednisone and skin rashes.
Rashes as a Side Effect
One important aspect to consider is that prednisone can actually cause skin rashes as a side effect. This may seem counterintuitive, as prednisone is often used to relieve symptoms of rashes. However, in some cases, individuals may develop a new rash or experience worsening of an existing rash while taking prednisone.
Immunosuppressive Properties
The connection between prednisone and skin rashes can be attributed to the medication's immunosuppressive properties. Prednisone works by suppressing the immune system, which can lead to a decreased ability to fight off infections and an increased susceptibility to skin problems. This can include skin rashes, as the immune response is not able to properly regulate inflammation and irritation.
Management and Prevention
If you are taking prednisone and develop a skin rash, it is important to consult with your healthcare provider. They can assess the rash and determine if it is a result of prednisone or another underlying factor. They may recommend adjusting the dosage of prednisone or exploring alternative treatment options.
It is also important to take steps to prevent skin rashes while taking prednisone. This can include keeping the skin clean and moisturized, avoiding irritants and allergens, and practicing good hygiene. Additionally, protecting the skin from excessive sun exposure and using sunscreen can help prevent skin rashes.
Conclusion
While prednisone can be an effective treatment for skin rashes, it is crucial to be aware of the potential link between prednisone and skin rashes. Understanding the possible side effects and taking preventative measures can help manage and minimize the risk of developing skin rashes while taking prednisone.
Understanding the Relationship between Prednisone and Skin Conditions
Prednisone is a medication that is commonly used to treat a variety of skin conditions. It belongs to a class of medications known as corticosteroids, which have anti-inflammatory effects on the body. This makes prednisone an effective treatment for skin conditions characterized by inflammation, such as eczema, psoriasis, and allergic reactions.
One of the main ways in which prednisone helps manage skin conditions is by reducing redness, itching, and swelling. When applied topically or taken orally, prednisone can help to calm the immune system, preventing it from overreacting to triggers that can lead to skin rashes. This results in a decrease in inflammation and an improvement in the appearance and comfort of the skin.
Prednisone and Eczema
Eczema is a common skin condition that is characterized by dry, itchy, and inflamed skin. Prednisone can be an effective treatment for eczema when other topical treatments have not been successful. By reducing inflammation and suppressing the immune system, prednisone can help to alleviate the symptoms of eczema and promote healing of the skin.
It is important to note that prednisone is typically used as a short-term treatment for eczema, as long-term use can lead to side effects. Your doctor will work with you to develop a treatment plan that includes prednisone, taking into account the severity of your eczema and any other underlying health conditions.
Prednisone and Psoriasis
Psoriasis is a chronic skin condition that is characterized by raised, red, and scaly patches of skin. Prednisone may be used in the treatment of psoriasis to help reduce inflammation and slow down the growth of skin cells. It is often used in combination with other medications or therapies for optimal results.
However, it is important to follow your doctor's instructions closely when using prednisone for psoriasis, as long-term use can have adverse effects on the body. Your doctor will monitor your progress and adjust your treatment plan as necessary to minimize side effects and maximize the benefits of prednisone.
In conclusion, prednisone can be an effective treatment for various skin conditions, including eczema and psoriasis. It helps to reduce inflammation, itching, and swelling, resulting in improved skin appearance and comfort. However, it is important to use prednisone under the guidance of a healthcare professional to ensure safe and effective use.
Common Types of Skin Rashes Caused by Prednisone
1. Acneiform eruption: Prednisone can cause an acne-like rash on the skin. This rash is characterized by small red bumps or pustules that may be filled with pus. The rash usually appears on the face, chest, and back.
2. Erythematous rash: Prednisone can also cause a red, patchy rash on the skin. This type of rash is often itchy and may be accompanied by inflammation and swelling. It can appear on any part of the body.
3. Photosensitivity: Prednisone can increase the skin's sensitivity to sunlight, leading to the development of a rash when exposed to the sun. This rash may be red, itchy, and blistering, and can appear on sun-exposed areas such as the face, neck, arms, and legs.
4. Contact dermatitis: Some people may develop an allergic reaction to prednisone, resulting in a contact dermatitis rash. This rash is typically red and itchy, and may appear in the areas where the medication was applied.
5. Hypersensitivity reaction: In rare cases, prednisone can cause a severe allergic reaction, known as a hypersensitivity reaction, which can manifest as a rash. This rash may be accompanied by other symptoms such as swelling, difficulty breathing, and dizziness.
6. Petechiae and purpura: Prednisone can also cause small red or purple spots on the skin, known as petechiae and purpura. These spots are caused by bleeding under the skin and may be a sign of a more serious condition.
7. Dry and thin skin: Prolonged use of prednisone can lead to dryness and thinning of the skin, making it more vulnerable to rashes and other skin irritations.
8. Stretch marks: Another common skin side effect of prednisone is the development of stretch marks, especially in areas where the skin is stretched, such as the abdomen, thighs, and buttocks.
9. Rash due to withdrawal: When prednisone is abruptly stopped or the dosage is significantly reduced, some individuals may experience a withdrawal rash. This rash may be accompanied by other withdrawal symptoms such as fatigue, muscle pain, and joint stiffness.
It is important to note that not everyone who takes prednisone will experience these skin rashes. The development and severity of rashes may vary depending on individual factors such as dosage, duration of treatment, and underlying medical conditions.
Identifying and Differentiating Prednisone-related Skin Rashes
Prednisone is a commonly prescribed medication that belongs to the class of corticosteroids. While it is effective in treating various medical conditions, one potential side effect of prednisone is the development of skin rashes. These rashes can vary in appearance and severity, making it important to identify and differentiate them from other skin conditions.
Common Types of Prednisone-related Skin Rashes
One common type of prednisone-related skin rash is known as steroid acne. This type of rash often appears as small, red bumps on the face, chest, and back. It is caused by the increased oil production in the skin due to the steroid medication. Steroid acne can be distinguished from other types of acne by its association with prednisone use and the absence of comedones.
Another type of prednisone-related skin rash is called perioral dermatitis. This rash typically affects the area around the mouth and appears as small, red bumps or pustules. It can be itchy and may be accompanied by dry or flaky skin. Perioral dermatitis can be mistaken for acne or allergic dermatitis, but it is important to identify its association with prednisone use.
Diagnosing Prednisone-related Skin Rashes
If you suspect that a skin rash is related to prednisone use, it is important to consult a healthcare professional for an accurate diagnosis. The healthcare provider may perform a physical examination of the rash and inquire about the medications being taken. In some cases, a skin biopsy or topical corticosteroid withdrawal test may be conducted to confirm the diagnosis.
During the evaluation, it is essential to differentiate the prednisone-related rash from other skin conditions such as allergic reactions, infections, or autoimmune disorders. The healthcare provider may ask about the timing of the rash onset in relation to prednisone initiation and may also consider the clinical presentation and response to discontinuing or adjusting the prednisone dosage.
Treatment and Management of Prednisone-related Skin Rashes
Once a prednisone-related rash has been diagnosed, the treatment approach will depend on the severity and specific type of rash. Mild rashes may resolve on their own once the prednisone dosage is tapered or discontinued. In some cases, topical medications like corticosteroid cream or antibiotics may be prescribed to manage the symptoms.
For more severe or persistent rashes, systemic treatment options such as oral corticosteroids or other immunosuppressant medications may be necessary. It is crucial to follow the healthcare provider's instructions and monitor the rash closely during treatment to ensure its resolution and prevent any complications.
In conclusion, identifying and differentiating prednisone-related skin rashes is essential for effective diagnosis and management. Working closely with a healthcare professional can help determine the underlying cause of the rash and guide appropriate treatment decisions.
Preventing and Managing Skin Rashes while on Prednisone
When taking prednisone, it is important to be aware of the potential side effect of skin rashes. These rashes can be itchy, uncomfortable, and can even lead to further complications if not properly managed. Fortunately, there are steps you can take to prevent and manage skin rashes while on prednisone.
1. Maintain good hygiene:
Keeping your skin clean and moisturized is essential in preventing skin rashes. Use gentle cleansers and avoid harsh soaps or products that may irritate your skin. After showering or bathing, pat your skin dry instead of rubbing and moisturize with a hypoallergenic lotion or cream.
2. Avoid triggers:
Identify any potential triggers that may worsen or cause skin rashes. Common triggers include certain fabrics, irritating chemicals or soaps, heat, and sweat. Try to avoid these triggers as much as possible to prevent flare-ups.
3. Protect your skin from the sun:
Prednisone can make your skin more sensitive to the sun's rays, which can increase the risk of developing a rash. Use broad-spectrum sunscreen with a high SPF and wear protective clothing, such as hats and long-sleeved shirts, when spending time outdoors.
4. Stay hydrated:
Drinking plenty of water can help keep your skin hydrated and prevent dryness, which can contribute to the development of rashes. Aim to drink at least 8 glasses of water per day to maintain optimal hydration.
5. Avoid scratching:
Although it may be tempting, avoid scratching your skin if you develop a rash. Scratching can worsen the rash and increase the risk of infection. Instead, apply a soothing cream or ointment and use cool compresses to alleviate any itching.
6. Follow the prescribed regimen:
It is important to take prednisone exactly as prescribed by your doctor. Do not skip doses or stop taking it abruptly, as this can lead to unpredictable effects on your skin and potentially worsen rashes. If you have any concerns or questions about your medication, consult with your healthcare provider.
By following these tips, you can help prevent and manage skin rashes while on prednisone. Remember to always consult with your healthcare provider if you experience any persistent or severe rashes, as they may need to adjust your medication or provide additional treatment.
Tips for Minimizing and Alleviating Prednisone-induced Skin Rashes
If you are taking prednisone and experiencing skin rashes as a side effect, there are several tips you can follow to minimize and alleviate the discomfort:
Avoid triggers
Identify any triggers that may be causing or worsening your skin rashes. These may include certain soaps, detergents, perfumes, or fabrics. Try to avoid these triggers as much as possible to prevent further irritation.
Keep your skin moisturized
Using a gentle, fragrance-free moisturizer can help to soothe and hydrate your skin. Apply it at least twice a day or as needed to keep your skin moisturized and prevent dryness and itching.
Avoid scratching
Itchy skin can be tempting to scratch, but this can worsen the rashes and lead to skin damage. Instead, try using a cold compress or applying a hydrocortisone cream to relieve the itching.
Stay hydrated
Drinking plenty of water can help to hydrate your skin from within and prevent dryness. Aim to drink at least 8 glasses of water a day to keep your skin healthy and moisturized.
Wear loose, breathable clothing
Tight or synthetic clothing can trap moisture and heat, leading to increased sweating and irritation. Opt for loose, breathable fabrics like cotton to allow your skin to breathe and minimize friction.
Consult your doctor
If your prednisone-induced skin rashes persist or worsen despite these measures, it is important to consult your doctor. They may be able to adjust your medication dosage or provide additional treatment options to alleviate your symptoms.
Remember, everyone's skin is different, so what may work for one person may not work for another. It's important to listen to your body and take the necessary steps to minimize and alleviate any discomfort or irritation caused by prednisone-induced skin rashes.
When to Seek Medical Attention for Prednisone-related Skin Rashes
If you are taking prednisone and develop a skin rash, it is important to pay attention to its appearance and any accompanying symptoms. While some rashes are mild and can be managed at home, others may require medical attention. It is important to know when to seek medical help to ensure proper diagnosis and treatment.
Severe Itching and Discomfort
If your skin rash is causing severe itching that is interfering with your daily activities or sleep, it may be a sign of a more serious reaction. In such cases, it is recommended to seek medical attention. Your healthcare provider can evaluate the rash and prescribe medications to relieve the itching and discomfort.
Worsening or Spreading Rash
If your rash is getting worse or spreading to other areas of your body despite home remedies or over-the-counter creams, it is advisable to consult a healthcare professional. They can determine if the rash is a result of an allergic reaction to prednisone or another underlying cause.
Persistent Rash
If your skin rash persists for more than a few days without any signs of improvement, it is important to seek medical attention. It could be an indication of an infection or an adverse drug reaction. Your healthcare provider can evaluate the rash and recommend appropriate treatment options.
Accompanying Symptoms
If your skin rash is accompanied by symptoms such as fever, difficulty breathing, swelling of the face or extremities, or any other concerning symptoms, it is crucial to seek immediate medical attention. These symptoms may indicate a severe allergic reaction, which requires prompt medical treatment.
In summary, if you experience severe itching, a worsening or spreading rash, a persistent rash, or accompanying symptoms, it is important to seek medical attention for your prednisone-related skin rash. Your healthcare provider can assess the rash and provide appropriate treatment options to relieve symptoms and address any underlying causes.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Can prednisone cause a skin rash"