Can prednisone cause diabetes type 2
Prednisone is a commonly prescribed medication used to treat a variety of conditions, including inflammatory diseases, autoimmune disorders, and certain types of cancer. While prednisone can be highly effective in managing these conditions, there is increasing evidence suggesting a potential link between the use of prednisone and an increased risk of developing type 2 diabetes.
Research studies have shown that prednisone can lead to elevated blood glucose levels, a key factor in the development of type 2 diabetes. This is because prednisone, as a corticosteroid, can interfere with the body's ability to properly regulate insulin and glucose metabolism. This disruption can result in insulin resistance, a condition in which the body becomes less responsive to the effects of insulin, leading to higher blood sugar levels.
Furthermore, prednisone use has been associated with weight gain, another risk factor for type 2 diabetes. The medication can cause an increase in appetite and fluid retention, leading to a higher calorie intake and a greater likelihood of developing obesity. Obesity is a known risk factor for type 2 diabetes, as excess body weight can impair insulin function and contribute to insulin resistance.
It is important for individuals taking prednisone to be aware of the potential risks and to closely monitor their blood sugar levels. If you are prescribed prednisone and have preexisting risk factors for type 2 diabetes, such as a family history of the disease or a sedentary lifestyle, it is especially important to discuss these concerns with your healthcare provider. They may recommend regular blood sugar testing, lifestyle modifications, or alternative treatment options to minimize the risk of developing type 2 diabetes.
Can prednisone raise the risk of type 2 diabetes?
Prednisone is a commonly prescribed medication used to treat a variety of inflammatory conditions. However, long-term use of prednisone has been associated with an increased risk of developing type 2 diabetes.
Studies have shown that prednisone can lead to insulin resistance, a condition in which the body's cells become less responsive to the hormone insulin, which is responsible for regulating blood sugar levels. Insulin resistance is a key factor in the development of type 2 diabetes, as it leads to higher blood sugar levels and can eventually result in the inability of the body to produce enough insulin to keep blood sugar levels under control.
In addition to insulin resistance, prednisone can also cause weight gain and an increase in appetite, both of which are risk factors for type 2 diabetes. Weight gain can lead to obesity, another major risk factor for the development of diabetes. The increased appetite can lead to overeating and a higher intake of calories, which can further contribute to weight gain and the development of diabetes.
If you are prescribed prednisone and have concerns about the potential risk of developing type 2 diabetes, it is important to discuss these concerns with your healthcare provider. They can provide you with information about the potential risks and benefits of the medication, and work with you to develop a plan for monitoring your blood sugar levels and managing any potential side effects.
Understanding the connection between prednisone and diabetes
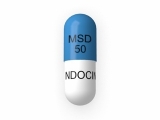
What is prednisone?
Prednisone is a medication commonly prescribed for the treatment of various inflammatory conditions, such as asthma, arthritis, and lupus. It belongs to a class of drugs called corticosteroids, which work by suppressing the immune system and reducing inflammation in the body.
Can prednisone increase the risk of developing type 2 diabetes?
Studies have suggested that the use of prednisone may increase the risk of developing type 2 diabetes, particularly in individuals who are already predisposed to the disease. Prednisone can cause a rise in blood sugar levels by decreasing the body's ability to efficiently use insulin, a hormone that helps regulate blood sugar. This can lead to insulin resistance and ultimately the development of type 2 diabetes.
How does prednisone affect blood sugar levels?
Prednisone can cause an increase in blood sugar levels through several mechanisms. It can promote glucose production in the liver, decrease glucose uptake by cells, and impair insulin secretion. This combination of factors can result in elevated blood sugar levels, especially in individuals with existing risk factors for diabetes, such as obesity or a family history of the disease.
What can be done to mitigate the risk?
If you are prescribed prednisone and are concerned about its potential impact on your blood sugar levels, there are several steps you can take to mitigate the risk. It is important to monitor your blood sugar levels regularly and work closely with your healthcare provider to adjust your diabetes management plan if needed. A healthy diet and regular exercise can also help manage blood sugar levels. Additionally, your healthcare provider may consider alternative medications or adjust your prednisone dosage to minimize the impact on blood sugar.
In conclusion
Prednisone, a commonly prescribed corticosteroid, may increase the risk of developing type 2 diabetes due to its effects on blood sugar regulation. It is important for individuals taking prednisone to be aware of this potential risk and work with their healthcare provider to manage their blood sugar levels effectively.
Risk factors for developing type 2 diabetes
Risk factors for developing type 2 diabetes can vary, but there are several common factors that can increase the likelihood of developing the condition.
Family history
A family history of type 2 diabetes can significantly increase the risk of developing the condition. Having a close relative, such as a parent or sibling, who has type 2 diabetes can increase the chances of developing the condition.
Obesity
Obesity is one of the most significant risk factors for developing type 2 diabetes. Excess weight, especially around the waist, increases the body's resistance to insulin, which can lead to high blood sugar levels and the development of diabetes.
Sedentary lifestyle
A sedentary lifestyle, characterized by a lack of physical activity, increases the risk of developing type 2 diabetes. Regular exercise helps the body to use insulin more efficiently and reduces the risk of insulin resistance.
Poor diet
A diet high in processed foods, sugary drinks, and unhealthy fats can contribute to the development of type 2 diabetes. Consuming a diet that lacks fruits, vegetables, and whole grains can increase the risk of the condition.
High blood pressure
Having high blood pressure can increase the risk of developing type 2 diabetes. High blood pressure can damage the blood vessels and hinder the body's ability to transport glucose, which can lead to elevated blood sugar levels.
Age
As individuals get older, the risk of developing type 2 diabetes increases. This is primarily due to lifestyle factors, such as decreased physical activity and poor dietary choices, which become more prevalent as people age.
It is important to note that having one or more of these risk factors does not guarantee the development of type 2 diabetes. However, being aware of these risk factors can help individuals make informed decisions about their lifestyle choices and take proactive steps to reduce their risk.
Effects of prednisone on blood sugar levels
Prednisone is known to have a significant impact on blood sugar levels. This medication, which belongs to a class of drugs called corticosteroids, can cause an increase in blood glucose levels, leading to a condition known as steroid-induced diabetes or drug-induced diabetes.
When prednisone is taken in high doses or for a long period of time, it can disrupt the normal functioning of insulin, a hormone that regulates blood sugar levels. It can result in insulin resistance, where the body's cells do not respond effectively to insulin. This can lead to higher blood sugar levels and eventually the development of type 2 diabetes.
Studies have shown that prednisone can also increase the production of glucose in the liver, further contributing to elevated blood sugar levels. Additionally, prednisone can impair the pancreas' ability to produce sufficient insulin, exacerbating the issue.
Individuals who are already at risk for developing type 2 diabetes, such as those with a family history or who are overweight, may be particularly susceptible to the effects of prednisone on blood sugar levels. It is important for healthcare providers to monitor blood glucose levels in these individuals while taking prednisone and to adjust their treatment plan accordingly.
In some cases, prednisone may be necessary for managing certain medical conditions. However, individuals taking prednisone should be aware of the potential risks on blood sugar levels and work closely with their healthcare provider to minimize these effects. Lifestyle modifications, such as healthy eating, regular exercise, and weight management, can also help mitigate the impact of prednisone on blood sugar levels.
Research findings on prednisone and diabetes risk
Prednisone use and diabetes prevalence
A number of studies have found a link between the use of prednisone and an increased risk of developing type 2 diabetes. One study, published in the Journal of Clinical Endocrinology and Metabolism, analyzed data from over 22,000 adults and found that the use of oral corticosteroids like prednisone was associated with a 70% increased risk of developing diabetes.
Similarly, a study conducted among patients with rheumatoid arthritis found that the use of prednisone was associated with a higher prevalence of diabetes compared to non-users. The researchers found that the risk of developing diabetes was dose-dependent, meaning that higher doses of prednisone were associated with a greater risk.
Mechanisms underlying the prednisone-diabetes association
Several mechanisms have been proposed to explain the association between prednisone use and increased diabetes risk. One possible mechanism is that prednisone can lead to insulin resistance, a condition where the body's cells become less responsive to the effects of insulin. Insulin resistance is a major contributing factor to the development of type 2 diabetes.
Another proposed mechanism is that prednisone can increase the release of glucose from the liver, leading to elevated blood sugar levels. Prednisone is known to stimulate the production of glucose in the liver through a process called gluconeogenesis.
Furthermore, prednisone has been found to impair the function of pancreatic beta cells, which are responsible for producing insulin. This can lead to a decrease in insulin production and contribute to the development of diabetes.
Recommendations for individuals taking prednisone
Given the increased risk of diabetes associated with prednisone use, individuals taking prednisone should be closely monitored for changes in blood sugar levels. Regular blood glucose testing may be necessary to ensure early detection of diabetes. In some cases, healthcare providers may recommend lifestyle modifications, such as adopting a healthy diet and increasing physical activity, to help mitigate the risk of diabetes.
It is also important for individuals taking prednisone to work closely with their healthcare providers to determine the most appropriate dosage and duration of treatment. In some cases, alternative medications may be considered to minimize the risk of developing diabetes.
Managing diabetes risk while taking prednisone
When taking prednisone, it is important to be aware of the potential risks associated with developing type 2 diabetes. Prednisone is a corticosteroid medication that is often prescribed to reduce inflammation and suppress the immune system. While this medication can be effective in treating a variety of conditions, it can also increase the risk of developing diabetes.
Monitoring blood sugar levels
To manage the risk of developing diabetes while taking prednisone, it is crucial to monitor blood sugar levels regularly. This can be done through finger prick tests or using a continuous glucose monitoring system. By keeping track of blood sugar levels, it is possible to detect any changes or abnormalities and take appropriate action.
Follow a healthy diet
A healthy diet is essential for managing diabetes risk while taking prednisone. This includes consuming a balanced mix of carbohydrates, proteins, and fats, as well as limiting the intake of sugary and processed foods. It is also important to incorporate plenty of fruits, vegetables, and whole grains into the diet, as they can help regulate blood sugar levels.
Engage in regular physical activity
Regular physical activity is key in managing diabetes risk while on prednisone. Exercise can help control blood sugar levels, improve insulin sensitivity, and maintain a healthy weight. Aim for at least 150 minutes of moderate-intensity aerobic activity per week, along with strength training exercises to build muscle mass.
Work closely with healthcare professionals
Managing diabetes risk while taking prednisone requires close collaboration with healthcare professionals. Regular check-ups and consultations with a healthcare team, including doctors, nurses, and dietitians, can help monitor blood sugar levels, adjust medications if necessary, and provide guidance on managing diabetes while on prednisone.
Summary: While prednisone can increase the risk of developing type 2 diabetes, there are strategies that can be employed to manage this risk. Regular monitoring of blood sugar levels, following a healthy diet, engaging in regular physical activity, and working closely with healthcare professionals are key in managing diabetes risk while taking prednisone.
Consulting your healthcare provider
It is important to consult your healthcare provider if you are concerned about the potential risk of developing type 2 diabetes while taking prednisone. They will be able to provide you with personalized advice and guidance based on your individual medical history and current health conditions.
Your healthcare provider will review your medical history and evaluate your risk factors for developing type 2 diabetes. They may also consider your current dose and duration of prednisone treatment, as well as other medications you may be taking.
During the consultation, your healthcare provider may discuss lifestyle modifications that can help reduce your risk of developing type 2 diabetes. This may include dietary changes, exercise recommendations, and monitoring your blood sugar levels. They may also recommend regular screenings for diabetes or other related conditions.
If you are already diagnosed with type 2 diabetes or have a family history of the condition, it is especially important to consult with your healthcare provider. They can work with you to develop a comprehensive management plan that takes into account the potential impact of prednisone on your blood sugar levels.
Remember, every individual is different, and the potential risk of developing type 2 diabetes while taking prednisone can vary. Consulting your healthcare provider is crucial in order to have a clear understanding of your specific risks and to receive appropriate guidance and support throughout your treatment.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube



Be the first to comment on "Can prednisone cause diabetes type 2"