Dangers of prednisone in the elderly
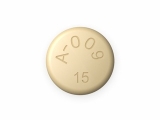
Prednisone is a commonly prescribed medication that belongs to a class of drugs known as corticosteroids. It is used to treat a variety of conditions, including inflammation, autoimmune disorders, and certain types of cancer. While prednisone can be highly effective in managing these conditions, it is important to be aware of the potential dangers it can pose, especially in older adults.
One of the major risks associated with prednisone use in the elderly is an increased susceptibility to infections. Prednisone works by suppressing the immune system, which can make it harder for the body to fight off bacteria, viruses, and other pathogens. This can lead to an increased risk of developing infections, such as pneumonia or urinary tract infections, which can be particularly dangerous for older individuals who may already have compromised immune systems.
Another concern with prednisone use in the elderly is the potential for adverse effects on bone health. Corticosteroids like prednisone can contribute to a loss of bone density, increasing the risk of osteoporosis and fractures. This is a significant concern for older adults, as they are already at an increased risk of developing these conditions due to age-related changes in bone metabolism. It is important for healthcare providers to carefully weigh the benefits and risks of prednisone treatment in elderly patients, taking into account their bone health status.
In addition, prednisone can also cause or exacerbate other common health issues in the elderly, such as diabetes, high blood pressure, and cataracts. These side effects can further complicate the management of chronic conditions and may require additional medical interventions. Healthcare providers need to closely monitor elderly patients on prednisone and make adjustments to their treatment plans as needed to minimize the risk of these complications.
Overall, while prednisone can be a valuable medication in the treatment of certain conditions, it is important to recognize and address the potential dangers it poses in the elderly population. By understanding the risks and closely monitoring elderly patients on prednisone, healthcare providers can help minimize the potential for adverse effects and ensure that the benefits of treatment outweigh the risks.
The Risks of Prednisone in the Elderly
As individuals age, their bodies become more susceptible to a variety of health issues, and the use of certain medications can present additional risks. One such medication is prednisone, a corticosteroid commonly prescribed to treat inflammatory conditions. While prednisone can be effective in managing these conditions, it is important to understand the potential risks, especially in elderly patients.
1. Increased risk of infections
Elderly individuals already have a weakened immune system, and the use of prednisone can further suppress immune function. This can lead to an increased risk of infections, including bacterial, viral, and fungal infections. It is essential for healthcare providers to closely monitor elderly patients on prednisone and promptly address any signs of infection to prevent complications.
2. Risk of osteoporosis and fractures
Prednisone can cause accelerated bone loss, leading to osteoporosis and an increased risk of fractures in the elderly. This is especially concerning as fractures in older adults can have serious consequences and hinder their overall mobility and quality of life. Healthcare professionals should consider prescribing calcium and vitamin D supplements, as well as monitor bone health in elderly patients taking prednisone.
3. Worsening of existing conditions
Prednisone can exacerbate certain pre-existing conditions that are common in the elderly, such as diabetes and hypertension. This can make managing these conditions more challenging and increase the risk of complications. Regular monitoring of blood glucose levels and blood pressure is crucial for elderly patients on prednisone to ensure proper management of these underlying conditions.
4. Adverse psychiatric effects
Elderly individuals are more susceptible to psychiatric side effects of prednisone, such as mood swings, irritability, and cognitive impairment. These effects can impact their overall well-being, behavior, and social interactions. It is important for healthcare providers to closely monitor elderly patients for any changes in mood or cognitive function while on prednisone and make adjustments to the dosage or consider alternative treatment options if needed.
In conclusion, while prednisone can be an effective treatment for various inflammatory conditions, including those commonly encountered in elderly patients, it is important to be aware of the potential risks associated with its use. Close monitoring, regular check-ups, and proactive management of potential side effects are essential to ensure the safety and well-being of elderly individuals receiving prednisone therapy.
Understanding the Potential Dangers
When it comes to using prednisone in the elderly, it is important to be aware of the potential dangers associated with this medication. Prednisone is a type of corticosteroid that is commonly prescribed to treat various conditions, such as inflammation, allergies, and autoimmune disorders. While it can be an effective treatment option, it also comes with a number of risks that need to be considered.
Increased Risk of Infection
One of the main dangers of prednisone in the elderly is an increased risk of infections. The immune system weakens as we age, and prednisone can further suppress the immune response, making it harder for the body to fight off infections. This can lead to an increased susceptibility to bacterial, viral, and fungal infections, which can be more severe and harder to treat in older adults.
Reduced Bone Density
Prolonged use of prednisone in the elderly can also lead to a reduction in bone density, increasing the risk of osteoporosis and fractures. Corticosteroids like prednisone can interfere with calcium absorption and bone formation, causing bone loss over time. Regular monitoring of bone density and the use of preventative measures, such as increased calcium intake and weight-bearing exercises, may help minimize this risk.
Hypertension and Fluid Retention
Another potential danger of prednisone in the elderly is the development of hypertension (high blood pressure) and fluid retention. Prednisone can cause an increase in sodium retention and fluid volume, leading to elevated blood pressure. This can be particularly problematic for seniors who may already have underlying cardiovascular conditions, putting them at a higher risk for heart attacks and strokes.
Gastrointestinal Side Effects
Prednisone use in the elderly can also result in a range of gastrointestinal side effects, including stomach ulcers, indigestion, and gastrointestinal bleeding. These side effects can be more severe in older adults, who may already have a compromised digestive system. Taking prednisone with food or using protective medications, such as proton pump inhibitors, may help alleviate these symptoms.
In conclusion, while prednisone can be an effective treatment option for certain conditions in the elderly, it is crucial to understand and minimize the potential dangers associated with its use. Close monitoring, regular check-ups, and taking preventative measures can help reduce the risks and ensure the well-being of older adults taking this medication.
Common Side Effects and Complications
Prednisone, a commonly prescribed corticosteroid, can cause a range of side effects and complications in the elderly population. It is important for healthcare professionals and caregivers to be aware of these potential risks and to take steps to minimize them.
One of the most common side effects of prednisone is weight gain. This occurs as the drug can cause an increase in appetite and a redistribution of fat to certain areas of the body. Weight gain can lead to a number of health problems, including diabetes, high blood pressure, and an increased risk of falls in the elderly.
Prednisone can also weaken the immune system, making elderly individuals more susceptible to infections. This can lead to frequent infections, such as urinary tract infections and respiratory infections, which can be more severe and difficult to treat in this population.
Another potential complication of prednisone use in the elderly is osteoporosis. Long-term use of corticosteroids can lead to bone loss and an increased risk of fractures. This is particularly concerning in the elderly, who may already have weaker bones due to age-related factors.
In addition, prednisone can cause mood changes and behavioral disturbances in some individuals. This can include symptoms such as irritability, anxiety, and depression. These psychological side effects can have a significant impact on an elderly individual's quality of life and overall well-being.
To minimize the risks and complications associated with prednisone use in the elderly, healthcare professionals should carefully monitor the dosage and duration of treatment. They should also explore other treatment options when possible and consider non-pharmacological interventions to manage symptoms. It is important to weigh the benefits of prednisone against the potential risks, particularly in the elderly population.
In conclusion, common side effects and complications of prednisone use in the elderly include weight gain, weakened immune system, osteoporosis, and mood changes. By being aware of these risks and taking steps to minimize them, healthcare professionals and caregivers can help ensure the safe and effective use of prednisone in elderly individuals.
Increased Risk of Infections
The use of prednisone in the elderly population can lead to an increased risk of infections. This is because prednisone is a corticosteroid medication that suppresses the immune system, making it harder for the body to fight off infections.
When the immune system is weakened, it becomes easier for bacteria, viruses, and other pathogens to enter the body and cause infections. The risk of developing infections such as respiratory tract infections, urinary tract infections, and skin infections is heightened in elderly individuals taking prednisone.
It is important for caregivers and healthcare providers to be vigilant for signs of infection in elderly patients on prednisone. Common symptoms such as fever, cough, difficulty breathing, urinary issues, and skin redness should not be ignored and should be reported to a healthcare professional.
To minimize the risk of infections, elderly patients on prednisone should take precautions such as practicing good hygiene, avoiding crowded places, and getting vaccinated against common infections, such as the flu and pneumonia. It is also important to follow the prescribed dosage and duration of prednisone treatment, as prolonged use can further weaken the immune system and increase the risk of infections.
Overall, understanding the increased risk of infections associated with prednisone in the elderly is crucial for ensuring their safety and well-being. Taking appropriate measures to minimize these risks can help in maintaining their health and preventing serious complications.
Impact on Bone Health and Fragility
Prednisone, a commonly prescribed corticosteroid medication, can have a negative impact on bone health and increase the risk of fractures and osteoporosis in the elderly. The long-term use of prednisone can cause bone loss, leading to a decrease in bone density and increased fragility.
One of the main mechanisms through which prednisone affects bone health is by suppressing the production of new bone. It inhibits the activity of osteoblasts, which are the cells responsible for building new bone. This imbalance between bone formation and bone resorption results in a net loss of bone mass over time.
In addition to its direct effects on bone formation, prednisone also promotes bone loss by impairing the absorption of calcium from the gastrointestinal tract and increasing the excretion of calcium through the kidneys. Calcium is an essential mineral for maintaining bone strength, and a deficiency can weaken the bones and increase the risk of fractures.
The use of prednisone in the elderly population is particularly concerning because aging itself is associated with a decline in bone density and an increased risk of osteoporosis. When combined with the bone-weakening effects of prednisone, this can lead to a significant increase in the risk of fractures and other bone-related complications.
To minimize the impact of prednisone on bone health, healthcare professionals may recommend the use of calcium and vitamin D supplements. These nutrients play a crucial role in maintaining bone strength and can help offset the negative effects of prednisone on bone health. In some cases, medications called bisphosphonates may also be prescribed to prevent or treat osteoporosis in individuals taking prednisone.
Regular weight-bearing exercise, such as walking or weightlifting, can also help strengthen bones and reduce the risk of fractures. Exercise stimulates the production of new bone and helps maintain bone density. Additionally, it is important for individuals on long-term prednisone therapy to undergo regular bone density scans to monitor their bone health and assess the need for further interventions.
Long-term Effects on Cognitive Function
Prednisone, a corticosteroid commonly prescribed to elderly patients, has been associated with long-term effects on cognitive function. Research has shown that long-term use of prednisone can lead to cognitive decline, including memory loss, confusion, and difficulty concentrating. These effects may be more pronounced in elderly individuals who are already at risk for cognitive impairment.
One study found that elderly patients who received prednisone for long periods of time had poorer cognitive performance compared to those who did not take the medication. The study also found that higher doses of prednisone were associated with greater cognitive decline. These findings suggest that the longer and higher the dosage of prednisone, the greater the impact on cognitive function.
The exact mechanism by which prednisone affects cognitive function is still unclear, but it is believed to involve several factors. One possibility is that prednisone may cause inflammation in the brain, leading to damage and dysfunction in the cognitive processes. Another possibility is that prednisone may interfere with the production and release of certain neurotransmitters that are essential for normal brain function.
To minimize the risk of long-term effects on cognitive function, it is important for healthcare providers to carefully consider the use of prednisone in elderly patients. Alternative treatments or lower doses of prednisone may be considered to reduce the potential impact on cognitive function. Regular monitoring of cognitive function and close observation of any changes or worsening symptoms is also crucial in elderly patients receiving prednisone therapy.
Minimizing the Risks: Best Practices and Alternatives
1. Proper Monitoring and Dosing
When prescribing prednisone to elderly patients, it is crucial to closely monitor their response and adjust the dosage as needed. Regular check-ups and lab tests can help identify any adverse effects and make necessary modifications to the treatment plan. By carefully titrating the dosage, healthcare professionals can minimize the risks associated with prednisone use in the elderly.
2. Use of the Lowest Effective Dose
To reduce the potential side effects of prednisone in elderly patients, it is advisable to prescribe the lowest effective dose. This means finding the dose that provides the desired therapeutic benefit while minimizing the risk of adverse reactions. Starting with a low dose and gradually increasing it if necessary can help strike the right balance.
3. Identifying and Managing Drug Interactions
Elderly patients often take multiple medications, increasing the risk of drug interactions. It is imperative to carefully evaluate the potential interactions between prednisone and the other drugs they are taking. Healthcare professionals should be aware of the medications being used and adjust the treatment plan accordingly to minimize any unwanted effects.
4. Promoting Bone Health
Prednisone use can lead to bone loss and increase the risk of fractures in the elderly. To counteract this effect, it is important to promote bone health through measures such as ensuring an adequate intake of calcium and vitamin D, regular weight-bearing exercise, and potentially using medications to prevent bone loss, as recommended by the healthcare provider.
5. Exploring Alternatives
In certain cases, it may be possible to explore alternative treatment options to minimize the use of prednisone in elderly patients. Non-steroidal anti-inflammatory drugs (NSAIDs), physical therapy, and other non-pharmacological interventions may be considered depending on the specific condition being treated. Discussing the available alternatives with the healthcare provider can help find the most suitable approach.
6. Educating Patients and Caregivers
Proper education of elderly patients and their caregivers is essential to ensure they understand the risks and benefits of prednisone use. Clear communication about the expected outcomes, potential side effects, and steps to take in case of any concerns can empower patients and help them make informed decisions. This education should be provided in a manner that is easily understandable and accessible to the elderly population.
In conclusion, minimizing the risks associated with prednisone use in the elderly requires a comprehensive approach that includes proper monitoring, the use of the lowest effective dose, managing drug interactions, promoting bone health, exploring alternative treatments, and patient education. By implementing these best practices, healthcare professionals can help mitigate the potential dangers while still providing effective treatment for elderly patients.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Dangers of prednisone in the elderly"