Prednisone dosing for eczema
Eczema is a common skin condition that causes dry, itchy, and inflamed patches on the skin. Prednisone is a medication that is often used to treat severe cases of eczema when other treatments have failed. Understanding the proper dosing of prednisone is essential to effectively managing the symptoms of eczema and minimizing side effects.
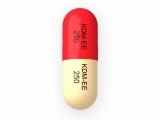
Prednisone is a type of corticosteroid that works by reducing inflammation and suppressing the immune system. When prescribed for eczema, prednisone is typically taken orally in tablet form. The dosage will vary depending on the severity of the eczema and the individual's response to the medication.
The initial dosing of prednisone for eczema is usually higher, known as an "initiation dose." This higher dose helps to quickly reduce inflammation and provide relief from itching. After a few weeks, the dosage is often tapered down to a lower "maintenance dose" to prevent rebound inflammation.
It is important to follow the prescribed dosing schedule and not to stop taking prednisone abruptly. Suddenly stopping prednisone can cause withdrawal symptoms and may lead to a flare-up of eczema. Your healthcare provider will work with you to determine the appropriate duration of treatment and tapering schedule based on your individual needs.
While prednisone can be a helpful treatment for severe eczema, it is important to be aware of and monitor for potential side effects. Some common side effects of prednisone include weight gain, increased appetite, mood changes, and difficulty sleeping. Long-term use of prednisone can also lead to more serious side effects such as osteoporosis, cataracts, and increased susceptibility to infections.
Overall, prednisone can be an effective medication for managing severe eczema when used properly and under the guidance of a healthcare professional. Understanding the dosing guidelines and potential side effects is crucial to ensure the safe and effective use of prednisone for eczema treatment.
The Basics of Prednisone Dosing for Eczema
Prednisone is a commonly prescribed medication for treating eczema flare-ups. It belongs to a class of drugs called corticosteroids, which work by reducing inflammation and suppressing the immune system. When used in appropriate doses, prednisone can help relieve the itching, redness, and swelling associated with eczema.
Dosage: The dosage of prednisone for eczema depends on various factors, including the severity of the flare-up, the individual's age, weight, and overall health condition. In general, the doctor will start with a low dose and gradually increase it if necessary. It is important to follow the prescribed dosage and not to exceed it without consulting a healthcare professional.
Duration of treatment: Prednisone is typically used for short-term treatment of eczema flare-ups. The duration of treatment may vary depending on the individual's response to the medication and the severity of the symptoms. In most cases, a course of prednisone can range from a few days to a few weeks. It is important to complete the full course of treatment as prescribed, even if the symptoms improve.
Possible side effects: Like any medication, prednisone can cause side effects. Common side effects include increased appetite, weight gain, fluid retention, mood changes, and difficulty sleeping. Long-term use of prednisone or high doses may increase the risk of more serious side effects, such as osteoporosis, high blood pressure, and infections. It is important to discuss the potential risks and benefits with a healthcare professional before starting treatment with prednisone.
Monitoring and follow-up: While on prednisone, regular monitoring and follow-up with a healthcare professional are necessary. This may include monitoring of blood pressure, blood sugar levels, and bone density. It is important to report any new or worsening symptoms to the doctor and to follow their advice regarding discontinuation or tapering of the medication.
Other considerations: Prednisone should be taken as prescribed and should not be stopped abruptly without medical supervision. Abrupt discontinuation can cause withdrawal symptoms and a flare-up of eczema. It is important to avoid alcohol and certain medications that can interact with prednisone. Additionally, taking the medication with food can help minimize stomach upset.
In conclusion, prednisone is an effective medication for managing eczema flare-ups. However, it should be used under medical supervision, with the prescribed dosage and duration. Regular monitoring and follow-up are important to ensure the medication's effectiveness and to minimize the risk of side effects.
Understanding Eczema and Its Symptoms
Eczema, also known as atopic dermatitis, is a chronic skin condition that affects millions of people worldwide. It is characterized by dry, itchy, and inflamed skin that can be red and swollen. Eczema often appears on the face, hands, feet, and bends of the elbows and knees. The exact cause of eczema is unknown, but it is believed to involve a combination of genetic and environmental factors.
One of the main symptoms of eczema is intense itchiness, which can be quite unbearable for those affected. Scratching the itchy skin can lead to further inflammation and even infections. In addition to itchiness, other common symptoms include redness, dryness, flaking, and thickening of the skin. These symptoms can vary in severity from mild to severe.
Eczema symptoms can occur in periodic flare-ups, where the skin becomes even more irritated and itchy. These flare-ups can be triggered by various factors, such as certain fabrics, soaps, detergents, and even stress. Identifying and avoiding triggers is an important part of managing eczema and reducing the frequency and severity of flare-ups.
It is important to seek medical advice if you suspect you have eczema or if the symptoms are severe or persistent. A healthcare professional can provide a proper diagnosis and recommend appropriate treatment options. By understanding eczema and its symptoms, individuals can better manage their condition and find relief from the discomfort it causes.
The Role of Prednisone in Eczema Treatment
Treating Acute Flares
Prednisone, a corticosteroid medication, plays a valuable role in the treatment of eczema, particularly during acute flares. When eczema flares up, it can cause severe itching, redness, and inflammation. Prednisone works by reducing inflammation and suppressing the immune system, which can help alleviate these symptoms.
However, it is important to note that prednisone is typically used as a short-term solution for managing severe eczema symptoms and should not be used as a long-term treatment.
Reducing Inflammation
One of the primary benefits of prednisone in eczema treatment is its ability to reduce inflammation. Inflammation is a key factor in the development and progression of eczema, and it is often responsible for the intense itching and discomfort associated with the condition. By suppressing inflammation, prednisone can provide relief and allow the skin to heal.
It is worth mentioning that prednisone may not be suitable for everyone, and its use should be carefully monitored by a healthcare professional to minimize potential side effects.
Managing Severe Symptoms
In cases where eczema symptoms are severe and cannot be effectively controlled through other treatments, prednisone may be prescribed. This medication can help manage the intense itching, redness, and swelling that often accompany severe eczema. It is typically used for a short duration to provide temporary relief and may be combined with other therapies for long-term management.
It is important to carefully follow the prescribed dosage and duration of prednisone treatment, as abruptly stopping the medication or taking it for an extended period can lead to withdrawal symptoms.
In summary, prednisone is a valuable tool in the treatment of eczema, particularly in managing acute flares and reducing inflammation. However, its use should be limited to short-term periods under the guidance of a healthcare professional to minimize potential side effects and ensure optimal results.
Factors to Consider When Prescribing Prednisone
1. Severity of the condition:
One of the first factors to consider when prescribing prednisone is the severity of the patient's eczema. Prednisone is a potent corticosteroid that is typically used for moderate to severe cases of eczema. If the eczema is mild or localized, alternative treatments may be more appropriate.
2. Duration of treatment:
Another important factor to consider is the duration of treatment. Prednisone is usually prescribed for short-term use, as long-term use can lead to potential side effects and complications. The duration of treatment should be based on the individual patient's needs and response to treatment.
3. Patient's medical history:
Before prescribing prednisone, it is important to consider the patient's medical history. Prednisone can interact with certain medications and may not be suitable for patients with certain medical conditions such as diabetes, osteoporosis, or high blood pressure. The patient's medical history should be thoroughly reviewed to ensure the safety and efficacy of prednisone treatment.
4. Potential side effects:
Prednisone can cause a range of side effects, including increased appetite, weight gain, mood changes, insomnia, and increased susceptibility to infections. It is important to consider the potential side effects and discuss them with the patient before prescribing prednisone. The benefits of treatment should be weighed against the potential risks.
5. Individual response to treatment:
Each patient may respond differently to prednisone, and the dosage may need to be adjusted accordingly. It is important to monitor the patient's response to treatment and make any necessary adjustments. Regular follow-up appointments should be scheduled to assess the effectiveness of prednisone and make any necessary changes to the treatment plan.
6. Gradual tapering of dosage:
When the decision is made to discontinue prednisone treatment, it is important to gradually taper the dosage to avoid withdrawal symptoms. Abruptly stopping prednisone can lead to adrenal insufficiency and other complications. The dosage should be gradually reduced over a period of time under medical supervision.
In conclusion, when prescribing prednisone for eczema, it is important to consider the severity of the condition, duration of treatment, patient's medical history, potential side effects, individual response to treatment, and the need for gradual tapering of dosage. This will help ensure the safe and effective use of prednisone for eczema management.
Tips for Proper Prednisone Dosing
1. Follow the prescribed dosage: It is important to carefully follow the dosage instructions provided by your healthcare provider. Prednisone is a powerful corticosteroid medication, and the dosage will depend on the severity of your eczema and your individual response to the drug. Taking the prescribed dose as directed is crucial for optimum results and to minimize the risk of side effects.
2. Take with food: Prednisone may cause stomach upset and other gastrointestinal side effects. To reduce the chances of these side effects, it is recommended to take prednisone with food or milk. This can help to protect the stomach lining and decrease irritation.
3. Stick to the schedule: Prednisone is usually prescribed as a daily medication, and it is important to take it at the same time each day. This will help to maintain consistent levels of the drug in your body and ensure its effectiveness.
4. Avoid sudden discontinuation: Prednisone should not be abruptly stopped without consulting your healthcare provider. Suddenly stopping the medication can cause withdrawal symptoms and may lead to a flare-up of your eczema. If you and your doctor decide to stop taking prednisone, your dosage will be tapered off slowly to minimize the risks.
5. Keep a symptom diary: It can be helpful to keep a record of your eczema symptoms while taking prednisone. Note any improvements, as well as any side effects you may experience. This information can provide important insights to your healthcare provider and help to adjust your treatment plan if necessary.
6. Stay hydrated: Prednisone can cause increased thirst and fluid retention. It is important to drink plenty of water while taking this medication to stay hydrated. Adequate hydration can also help to flush out any toxins and minimize the risk of certain side effects.
7. Follow up with your healthcare provider: Regular check-ups with your healthcare provider are important while taking prednisone. These appointments allow your doctor to assess your progress, monitor any potential side effects, and make any necessary adjustments to your treatment plan.
8. Educate yourself about prednisone: Understanding how prednisone works, its potential side effects, and its role in managing your eczema can help you make informed decisions about your treatment. Talk to your healthcare provider, do independent research, and ask questions to ensure you have a good understanding of the medication and its benefits and risks.
Potential Side Effects of Prednisone
1. Increased risk of infection:
One potential side effect of prednisone is an increased risk of infection. This is because prednisone works by suppressing the immune system, which can make it harder for the body to fight off infections. It is important to take precautions to avoid getting sick, such as washing your hands regularly and avoiding contact with people who are ill.
2. Weight gain:
Prednisone can cause weight gain due to its effect on the body's metabolism. This weight gain is often due to an increase in appetite and water retention. It is important to maintain a healthy diet and exercise regularly to help manage weight gain while taking prednisone.
3. Changes in mood and behavior:
Prednisone can also affect mood and behavior. Some people may experience irritability, mood swings, or even depression while taking prednisone. It is important to monitor any changes in mood and discuss them with your healthcare provider.
4. Osteoporosis:
Prolonged use of prednisone can lead to thinning of the bones, known as osteoporosis. This can increase the risk of fractures. If you are using prednisone long-term, your healthcare provider may recommend calcium and vitamin D supplements or other medications to help prevent bone loss.
5. Elevated blood sugar levels:
Prednisone can cause an increase in blood sugar levels, which can be problematic for individuals with diabetes or those at risk for developing diabetes. If you have diabetes, it is important to closely monitor your blood sugar levels while taking prednisone and adjust your diabetes medication as needed.
6. Adrenal insufficiency:
Prolonged use of prednisone can suppress the function of the adrenal glands, which produce important hormones. This can lead to a condition called adrenal insufficiency, where the body is unable to produce enough cortisol. If you have been taking prednisone for an extended period of time, it is important to gradually reduce the dosage under the guidance of your healthcare provider to allow your adrenal glands to recover.
7. Eye problems:
Some individuals may experience eye problems while taking prednisone, such as cataracts or glaucoma. It is important to have regular eye exams while taking prednisone to monitor for any changes in vision or eye health.
It is important to note that not everyone will experience these side effects, and the severity of side effects can vary from person to person. It is important to closely follow your healthcare provider's instructions and communicate any concerns or side effects you may be experiencing while taking prednisone.
Consulting Your Doctor for Prednisone Dosing
1. Understand your eczema condition:
Before consulting your doctor for prednisone dosing, it is important to have a clear understanding of your eczema condition. This includes knowing the severity of your symptoms, any previous treatments you have tried, and any triggers or factors that aggravate your eczema. By having this information, you can provide your doctor with accurate details about your condition and help them determine the right prednisone dosage for you.
2. Schedule an appointment with your doctor:
Make an appointment with your primary care physician or dermatologist to discuss your eczema and prednisone dosing. It is important to consult a healthcare professional who has experience in treating eczema and prescribing medications like prednisone. During the appointment, be prepared to provide a detailed medical history and discuss your eczema symptoms, triggers, and previous treatments. This will help your doctor make an informed decision about the appropriate prednisone dosage.
3. Ask questions and voice concerns:
During your appointment, don't hesitate to ask questions about prednisone dosing. Seek clarification on any uncertainties or concerns you may have. Prednisone is a powerful medication with potential side effects, so it is crucial to understand the risks and benefits associated with its use. Your doctor can provide you with information about potential side effects, how to minimize them, and any alternative treatment options that may be available.
4. Follow your doctor's instructions:
Once your doctor has determined the appropriate prednisone dosage for your eczema, it is important to strictly follow their instructions. Take the medication exactly as prescribed, including the dosage and duration. Do not stop or adjust the dosage without consulting your doctor first, as this can have adverse effects on your condition. If you experience any side effects or have concerns while taking prednisone, contact your doctor for further guidance.
5. Regularly monitor your condition:
After starting prednisone treatment, it is important to regularly monitor your eczema condition and report any changes or concerns to your doctor. Keep track of your symptoms, including their severity and frequency. This will help your doctor assess the effectiveness of the prednisone dosage and make any necessary adjustments to your treatment plan. Additionally, inform your doctor about any new triggers or factors that may be affecting your eczema.
Consulting your doctor for prednisone dosing is an essential step in managing your eczema. By working closely with your healthcare professional, you can ensure that the prednisone dosage is tailored to your specific needs and maximize the benefits of the medication while minimizing potential side effects.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Prednisone dosing for eczema"