Prednisone withdrawal skin rash
Prednisone is a commonly prescribed medication for the treatment of various inflammatory conditions. However, stopping the use of prednisone abruptly can lead to withdrawal symptoms, including a skin rash. This article explores the symptoms, causes, and treatment options for prednisone withdrawal skin rash.
When a person has been taking prednisone for an extended period, their body becomes dependent on the medication to regulate inflammation. Suddenly stopping or reducing the dosage of prednisone can disrupt this balance and cause withdrawal symptoms, such as skin rash.
The symptoms of prednisone withdrawal skin rash can vary from person to person. Some common symptoms include redness, itching, and the appearance of small bumps or blisters on the skin. In severe cases, the rash may also be accompanied by swelling and pain.
There are several possible causes for prednisone withdrawal skin rash. One possibility is that the sudden reduction or cessation of prednisone leads to a rebound effect, where the body overreacts to even minor triggers and produces an inflammatory response. Another possible cause is that the immune system, which may have been suppressed by long-term prednisone use, becomes overactive once the medication is stopped, leading to the development of a skin rash.
Fortunately, there are various treatment options available for prednisone withdrawal skin rash. In mild cases, over-the-counter topical creams or ointments containing hydrocortisone may provide relief. For more severe cases, a dermatologist may prescribe stronger medications, such as corticosteroid creams or oral antihistamines, to alleviate the symptoms. It is important to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan.
In conclusion, prednisone withdrawal can lead to the development of a skin rash. The symptoms can vary from person to person and may include redness, itching, and the appearance of bumps or blisters. The rash can be caused by the body's overreaction to minor triggers or an overactive immune system. Treatment options range from over-the-counter creams to prescription medications, depending on the severity of the rash. It is always important to seek medical advice for proper diagnosis and treatment.
Symptoms of Prednisone Withdrawal Skin Rash
When a person stops taking prednisone, they may experience a skin rash as part of the withdrawal symptoms. This rash can present with various symptoms and can vary in severity. Here are some common symptoms of prednisone withdrawal skin rash:
- Redness: The affected area may appear red and inflamed.
- Itching: The rash may cause intense itching and discomfort.
- Bumps or blisters: Small bumps or blisters may develop on the skin.
- Scaling: The rash may cause the skin to become dry and scaly.
- Swelling: In some cases, the affected area may become swollen.
- Pain or tenderness: The rash may be painful or tender to the touch.
In addition to these symptoms, a prednisone withdrawal skin rash may also cause other general symptoms such as fatigue, headache, and muscle aches. It is important to note that the severity and duration of the rash can vary from person to person.
Visible Skin Rashes
Skin rashes are a common manifestation of prednisone withdrawal. These rashes can vary in appearance and severity, and may cause discomfort and itching. It is important to seek medical attention if you experience any visible skin rashes during prednisone withdrawal.
One type of visible skin rash that may occur is erythema. This rash is characterized by redness and inflammation of the skin. It can appear as small patches, larger areas, or even as a widespread rash. Erythema can be itchy and uncomfortable, and may be accompanied by a burning sensation.
Another type of skin rash that may occur is urticaria, also known as hives. Urticaria is characterized by raised, red, and itchy bumps on the skin. These bumps can range in size and may appear in clusters or as individual lesions. Urticaria can be triggered by various factors, such as allergens or stress.
In some cases, prednisone withdrawal may cause a rash known as dermatitis. Dermatitis is an inflammatory skin condition that can cause redness, itching, and even blistering or peeling of the skin. The rash may be localized or spread over a larger area of the body. It is important to seek medical attention if you suspect you have dermatitis during prednisone withdrawal.
Summary: Visible skin rashes are a common symptom of prednisone withdrawal. These rashes can include erythema, urticaria, and dermatitis, and may cause discomfort, itching, and inflammation of the skin. It is important to seek medical attention if you experience any visible skin rashes during prednisone withdrawal.
Severe Itching and Irritation
One of the most common symptoms of prednisone withdrawal is severe itching and irritation of the skin. This can be extremely uncomfortable and may lead to scratching, which can further damage the skin and cause additional irritation.
The itching and irritation experienced during withdrawal from prednisone is typically due to the body's adjustment to not having the medication. Prednisone is a corticosteroid that suppresses the immune system and reduces inflammation, so when it is suddenly stopped, the body may overcompensate and produce excess inflammatory substances. This can result in a histamine release, leading to itching and irritation.
Some individuals may experience a more severe form of itching known as pruritus. This can be so intense that it disrupts daily activities and sleep. Itching and irritation may be localized to certain areas of the body or may be widespread.
There are several approaches to managing severe itching and irritation during prednisone withdrawal. One option is to use over-the-counter antihistamines, which can help alleviate itching. Topical creams and ointments containing hydrocortisone may also be effective in reducing inflammation and relieving itching.
Additionally, it is important to keep the skin well-moisturized to prevent further drying and irritation. Using gentle, fragrance-free skincare products and avoiding hot showers or baths can help maintain skin health.
If severe itching and irritation persist or worsen, it is important to consult a healthcare professional. They may recommend prescription-strength medications or other treatments to provide relief. It is also important to address the underlying cause of the withdrawal symptoms and work closely with a healthcare professional to safely taper off prednisone.
Causes of Prednisone Withdrawal Skin Rash
The skin rash that can occur after withdrawing from prednisone, a corticosteroid medication, can have several causes. One possible cause is the rebound effect, where the body overreacts to the withdrawal of the medication, leading to inflammation and skin rash. This rebound effect is more likely to occur if prednisone was used at higher doses or for a longer period of time.
Another cause of prednisone withdrawal skin rash is the disruption of the body's natural hormone production. Prednisone suppresses the production of certain hormones, such as cortisol, which are essential for maintaining balance in the body. When prednisone is abruptly stopped, the body may have difficulty readjusting its hormone levels, leading to skin rash as a result of this hormonal imbalance.
In some cases, the skin rash may be a manifestation of an underlying condition or disease that was being treated with prednisone. Prednisone is often prescribed to manage autoimmune disorders, such as lupus or rheumatoid arthritis, and withdrawal from the medication can result in a flare-up of these conditions, leading to skin rash.
Additionally, prednisone withdrawal skin rash can occur due to the body's immune system being suppressed by the medication. Prednisone reduces inflammation by suppressing the immune system, and withdrawal of the medication can cause the immune system to become overactive, leading to an inflammatory response and skin rash.
It is important to note that the specific cause of prednisone withdrawal skin rash may vary from person to person, and it is best to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
Hormonal Imbalance
Hormonal imbalance refers to when there is an abnormality in the levels of hormones in the body. Hormones play a crucial role in regulating various bodily functions and processes, including growth, metabolism, reproduction, and mood. When the balance of hormones is disrupted, it can lead to a wide range of symptoms and health issues.
Causes
There are several factors that can contribute to hormonal imbalance. One common cause is stress, as it can disrupt the normal production and regulation of hormones in the body. Other causes include certain medical conditions, such as polycystic ovary syndrome (PCOS) and thyroid disorders. Additionally, hormonal imbalance can be triggered by lifestyle factors, such as poor diet, lack of exercise, and inadequate sleep.
Symptoms
The symptoms of hormonal imbalance can vary depending on the specific hormones that are affected. Common symptoms include fatigue, weight gain or loss, changes in appetite, mood swings, irregular periods, infertility, and acne. In some cases, hormonal imbalance can also lead to more serious health conditions, such as diabetes or osteoporosis.
Treatment
Treating hormonal imbalance often involves identifying and addressing the underlying cause. This may involve making lifestyle changes, such as adopting a healthy diet and exercise routine, managing stress levels, and getting enough sleep. In some cases, hormonal therapy or medication may be necessary to restore hormone levels to a normal range. It is important to consult with a healthcare professional to determine the most appropriate treatment plan.
Immune System Dysfunction
Immune system dysfunction refers to a condition where the body's immune system does not function properly. This can lead to various health issues and make the body more susceptible to infections and diseases. There are several factors that can contribute to immune system dysfunction, including genetic predisposition, environmental factors, and certain medications.
Genetic Predisposition: Some individuals may inherit genes that make their immune system more prone to dysfunction. This can lead to a weakened immune response and a higher risk of developing autoimmune disorders or allergies.
Environmental Factors: Exposure to certain environmental factors, such as pollutants, toxins, or pathogens, can disrupt the normal functioning of the immune system. This can result in an overactive immune response or a weakened immune system, both of which can lead to health problems.
Medications: Certain medications, such as corticosteroids or immunosuppressants, can interfere with the immune system. While these medications may be necessary to treat certain conditions, they can also have side effects that weaken the immune system or cause it to malfunction.
Effects of Immune System Dysfunction: Immune system dysfunction can manifest in various ways, depending on the specific condition or underlying cause. Some common symptoms include frequent infections, chronic inflammation, allergies, and autoimmune disorders. In severe cases, immune system dysfunction can lead to life-threatening conditions, such as organ failure or an increased susceptibility to cancer.
Early detection and prompt treatment of immune system dysfunction are important to minimize the impact on overall health. This may involve lifestyle modifications, such as reducing exposure to environmental toxins, eating a balanced diet, and adopting healthy habits. In some cases, medication or other treatments may be necessary to manage the underlying cause of immune system dysfunction. Consulting with a healthcare professional is essential for accurate diagnosis and effective management of the condition.
Treatment for Prednisone Withdrawal Skin Rash
When experiencing a skin rash due to prednisone withdrawal, it is important to seek medical attention for proper diagnosis and treatment. The specific treatment plan will depend on the severity of the rash and the individual's medical history.
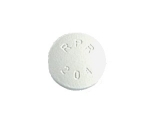
1. Topical Steroids
One common treatment option for prednisone withdrawal skin rash is the use of topical steroids. These creams or ointments contain steroid ingredients that can help reduce inflammation and relieve itching. It is important to follow the instructions provided by the healthcare professional regarding the frequency and duration of use.
2. Antihistamines
In some cases, antihistamines may be prescribed to help alleviate itching and reduce allergic reactions associated with the skin rash. These medications work by blocking the action of histamines in the body, which are released during an allergic reaction.
3. Moisturizers
Using moisturizers can help soothe the skin and prevent further irritation. Look for moisturizers that are fragrance-free and gentle on the skin. Apply the moisturizer after bathing or as directed by the healthcare professional.
4. Avoiding Triggers
Identifying and avoiding triggers that may worsen the skin rash is an important part of the treatment plan. This may include avoiding certain fabrics, skincare products, or environmental factors that can irritate the skin.
5. Gradual tapering of prednisone
In cases where the skin rash is a result of prednisone withdrawal, a healthcare professional may recommend a gradual tapering of the medication to help minimize withdrawal symptoms and reduce the likelihood of a rash occurring.
Disclaimer: This article is for informational purposes only and should not replace the advice of a healthcare professional. Always consult with a healthcare professional for proper diagnosis and treatment of prednisone withdrawal skin rash.
Topical Steroid Creams
What are topical steroid creams?
Topical steroid creams are medications that are applied to the skin to reduce inflammation and treat various skin conditions. They contain corticosteroids, which are powerful anti-inflammatory drugs.
How do topical steroid creams work?
Topical steroid creams work by reducing inflammation in the skin. They bind to specific receptors in the skin cells, which then inhibits the production of inflammatory chemicals. This helps to relieve symptoms such as itching, redness, and swelling.
When are topical steroid creams used?
Topical steroid creams are commonly used to treat skin conditions such as eczema, dermatitis, psoriasis, and allergic reactions. They can also be used to reduce inflammation and itching caused by insect bites or rashes.
How should topical steroid creams be used?
It is important to follow the instructions provided by your healthcare provider or the information leaflet that comes with the medication. Topical steroid creams should generally be applied thinly and evenly to the affected area of the skin. It is usually recommended to wash and dry the skin before applying the cream. The frequency of application and duration of treatment will depend on the specific condition being treated.
What are the potential side effects of topical steroid creams?
While topical steroid creams are generally safe when used as directed, they can potentially cause side effects. These may include thinning of the skin, skin discoloration, acne, increased hair growth, and skin infections. It is important to use these creams sparingly and only as directed by a healthcare professional.
Conclusion
Topical steroid creams are effective medications for reducing inflammation and treating various skin conditions. However, they should be used cautiously and under the guidance of a healthcare professional to minimize the risk of potential side effects.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Prednisone withdrawal skin rash"