Psoriatic arthritis and prednisone
Psoriatic arthritis is an inflammatory condition that affects individuals who have psoriasis, a chronic skin condition. It is characterized by joint pain, swelling, and stiffness, and can significantly impact the quality of life for those affected. While there is no cure for psoriatic arthritis, there are various treatment options available to manage symptoms and improve overall well-being.
Prednisone is a corticosteroid medication that is commonly prescribed to individuals with psoriatic arthritis to reduce inflammation and alleviate pain. It works by suppressing the immune system and decreasing the production of inflammatory substances. While prednisone can provide significant relief from symptoms, it is important to understand the potential benefits and risks associated with its use.
One of the benefits of prednisone is its ability to quickly reduce inflammation, which can lead to a noticeable decrease in joint pain and swelling. This can significantly improve mobility and allow individuals to engage in activities that may have been previously limited by their symptoms. Additionally, prednisone can help to prevent or minimize joint damage, which is especially important in individuals with severe psoriatic arthritis.
However, it is important to be aware of the potential risks and side effects of long-term prednisone use. These can include weight gain, increased risk of infections, bone loss, and mood changes. To minimize these risks, doctors often prescribe prednisone at the lowest effective dose for the shortest duration possible. Regular monitoring and close communication with a healthcare provider are essential to ensure that the benefits of prednisone outweigh its potential risks.
Psoriatic Arthritis and Prednisone
The Benefits of Prednisone for Psoriatic Arthritis
Prednisone is a corticosteroid medication commonly used to treat inflammation in various conditions, including psoriatic arthritis. It works by reducing the immune response that contributes to joint inflammation, swelling, and pain.
Prednisone can provide significant relief for psoriatic arthritis symptoms, such as joint pain, stiffness, and swelling. It can help improve mobility and quality of life for individuals with this chronic inflammatory condition.
The Risks of Prednisone for Psoriatic Arthritis
While prednisone can be an effective treatment option, it is important to be aware of the potential risks and side effects associated with long-term use.
Prolonged use of prednisone can increase the risk of osteoporosis, cataracts, weight gain, high blood pressure, and diabetes. It can also weaken the immune system, making individuals more susceptible to infections.
It is crucial for individuals taking prednisone for psoriatic arthritis to work closely with their healthcare provider to monitor and manage these potential risks. Regular check-ups, bone density tests, and blood pressure monitoring may be recommended.
Weighing the Benefits and Risks
Deciding to use prednisone for psoriatic arthritis is a complex decision that depends on the severity of symptoms, individual health history, and other treatment options. It is important to have an open and honest discussion with a healthcare provider to weigh the potential benefits against the risks.
In some cases, the short-term use of prednisone may be necessary to manage severe flare-ups and provide immediate relief. However, long-term use should be carefully considered, and alternative treatment options, such as disease-modifying antirheumatic drugs (DMARDs) or biologic medications, may be explored.
Ultimately, the goal is to find the most effective and safest treatment approach to manage psoriatic arthritis symptoms, minimize long-term risks, and improve overall quality of life.
Understanding the Benefits and Risks
Benefits of Prednisone for Psoriatic Arthritis
Prednisone, a corticosteroid medication, can provide several benefits for individuals with psoriatic arthritis. It can help reduce inflammation and swelling in the joints, which can relieve pain and stiffness. This can lead to improved mobility and a better quality of life. Prednisone can also help manage other symptoms associated with psoriatic arthritis, such as skin rashes and fatigue.
Risks of Prednisone for Psoriatic Arthritis
While prednisone can be beneficial, it is important to understand the risks associated with its use. Prolonged use of prednisone can lead to various side effects, including weight gain, high blood pressure, and mood changes. It can also weaken the immune system, making individuals more susceptible to infections. Additionally, long-term use of prednisone can contribute to the development of osteoporosis, a condition characterized by weak and fragile bones.
Weighing the Benefits and Risks
When considering the use of prednisone for psoriatic arthritis, it is crucial to weigh the potential benefits against the risks. Each individual's situation is unique, and it is important to work closely with a healthcare provider to determine the best treatment approach. Factors such as the severity of symptoms, overall health, and lifestyle should be taken into consideration. Alternatives to prednisone, such as other medications or lifestyle changes, may also be explored to find the most effective and safe treatment plan.
Monitoring and Managing Risks
If prednisone is prescribed for psoriatic arthritis, it is essential to regularly monitor and manage the associated risks. This may involve regular check-ups with a healthcare provider to assess any potential side effects or complications. It is important to follow the prescribed dosage and duration of prednisone use and to gradually taper off the medication as directed. A healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking and excessive alcohol consumption, can also help mitigate the risks associated with prednisone use.
What is Psoriatic Arthritis?
Psoriatic arthritis is a chronic inflammatory condition that affects both the skin and the joints. It is a type of arthritis that occurs in some people with psoriasis, a chronic skin condition characterized by red, scaly patches on the skin. Psoriatic arthritis can cause pain, swelling, and stiffness in the joints, along with symptoms such as fatigue, nail changes, and eye inflammation. The exact cause of psoriatic arthritis is unknown, but it is believed to be a combination of genetic and environmental factors.
Psoriatic arthritis can affect any joint in the body, including the hands, feet, knees, and spine. The severity of symptoms can vary widely from person to person, with some experiencing mild, intermittent discomfort and others experiencing more severe, persistent pain. In addition to joint symptoms, psoriatic arthritis can also cause inflammation in other parts of the body, such as the tendons and ligaments, leading to symptoms such as heel pain and stiffness in the back or neck.
Treatment for psoriatic arthritis aims to control symptoms, prevent joint damage, and improve quality of life. This typically involves a combination of medications, including nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation, disease-modifying antirheumatic drugs (DMARDs) to slow disease progression, and biologics, which target specific components of the immune system. In some cases, prednisone, a type of corticosteroid, may be prescribed to help temporarily reduce inflammation and provide relief during flare-ups.
Exploring the Symptoms and Causes
Psoriatic arthritis is a chronic inflammatory condition that affects individuals who have psoriasis, a skin disorder characterized by red, scaly patches. The symptoms of psoriatic arthritis can vary from person to person, but commonly include joint pain, stiffness, and swelling. In some cases, individuals may also experience fatigue, nail changes, and eye inflammation.
The exact cause of psoriatic arthritis is unknown, but it is believed to be related to an abnormal immune response. The immune system mistakenly attacks healthy cells and tissues, leading to inflammation in the joints. Genetic factors are also thought to play a role in the development of psoriatic arthritis, as the condition tends to run in families. Additionally, certain environmental triggers, such as infections or injuries, may activate the immune response and contribute to the onset of psoriatic arthritis.
Psoriatic arthritis can be diagnosed through a combination of physical examination, medical history, and imaging tests. Doctors will look for signs of joint inflammation, such as redness, warmth, and swelling. They may also order blood tests to check for markers of inflammation in the body. X-rays and other imaging tests may be used to assess the extent of joint damage and rule out other conditions.
Managing the symptoms of psoriatic arthritis often involves a combination of medications, lifestyle modifications, and physical therapy. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce pain and inflammation. Disease-modifying antirheumatic drugs (DMARDs) and biologic medications can help slow down the progression of the disease and prevent joint damage. In some cases, corticosteroids like prednisone may be used for short-term relief of severe symptoms.
Treating Psoriatic Arthritis
Psoriatic arthritis is a chronic condition that affects both the skin and the joints. It can cause pain, stiffness, swelling, and fatigue, making it difficult for individuals to carry out their daily activities. Fortunately, there are several treatment options available to help manage the symptoms and improve quality of life for those with psoriatic arthritis.
Medications
One of the main treatment options for psoriatic arthritis is the use of medications. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation, while disease-modifying antirheumatic drugs (DMARDs) can slow down the progression of the disease. In some cases, corticosteroids may be prescribed to help manage severe symptoms.
Biologic agents, such as tumor necrosis factor (TNF) inhibitors, can also be effective in treating psoriatic arthritis. These medications target specific components of the immune system to reduce inflammation and alleviate symptoms. However, they may have potential side effects and should be used under the guidance of a healthcare professional.
Lifestyle Changes
In addition to medication, certain lifestyle changes can play a crucial role in managing psoriatic arthritis. Regular exercise, such as low-impact activities like swimming or cycling, can help improve joint mobility and reduce pain. Maintaining a healthy weight can also alleviate stress on the joints.
A balanced diet rich in fruits, vegetables, and omega-3 fatty acids can provide essential nutrients to support overall joint health. Some studies suggest that a gluten-free diet may also be beneficial for individuals with psoriatic arthritis, although more research is needed to establish a firm connection.
Additional Therapies
In some cases, individuals with psoriatic arthritis may benefit from additional therapies. Physical therapy can help improve joint function and flexibility through specialized exercises and techniques. Occupational therapy can assist with adapting daily activities to reduce strain on the joints.
In more severe cases, surgery may be considered to repair or replace damaged joints. This option is typically reserved for individuals who have not found relief through other treatments and have significant joint damage.
It's important for individuals with psoriatic arthritis to work closely with their healthcare team to develop a personalized treatment plan. Regular monitoring and adjusting of medications and therapies may be necessary to ensure the best possible outcomes. With the right treatment approach, individuals with psoriatic arthritis can effectively manage their condition and improve their quality of life.
Options for Managing Joint Pain and Inflammation
Psoriatic arthritis can cause significant joint pain and inflammation, making it important to find effective ways to manage these symptoms. Fortunately, there are several options available:
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs are commonly used to relieve joint pain and reduce inflammation. They work by inhibiting the production of certain chemicals in the body that cause pain and inflammation. Common NSAIDs include ibuprofen, naproxen, and diclofenac. It is important to follow the recommended dosage and talk to your doctor about potential side effects.
2. Disease-Modifying Antirheumatic Drugs (DMARDs)
DMARDs are a type of medication that can slow down the progression of psoriatic arthritis and help manage joint pain and inflammation. They work by targeting the immune system and reducing inflammation. Methotrexate, sulfasalazine, and leflunomide are examples of DMARDs commonly used in the treatment of psoriatic arthritis. It is important to discuss potential risks and benefits with your healthcare provider.
3. Corticosteroids
Corticosteroids, such as prednisone, may be prescribed to manage severe joint pain and inflammation in psoriatic arthritis. These medications work by reducing inflammation and suppressing the immune system. However, they may have significant side effects when used long-term, so they are typically used for short-term relief. Regular monitoring and adjustment of the dosage is important when taking corticosteroids.
4. Biologic Response Modifiers
Biologic response modifiers, also known as biologics, are a newer class of medications that target specific proteins involved in the immune response. They can be effective in reducing joint pain and inflammation in psoriatic arthritis. Examples of biologic medications used in the treatment of psoriatic arthritis include adalimumab, infliximab, and ustekinumab. These medications are typically administered by injection or infusion and require regular monitoring.
5. Physical Therapy and Exercise
Physical therapy can be beneficial for managing joint pain and improving mobility in psoriatic arthritis. A physical therapist can provide exercises and techniques to reduce pain, improve joint function, and strengthen the muscles supporting the joints. Regular exercise, such as low-impact activities like swimming or cycling, can also help maintain joint flexibility and reduce stiffness.
6. Lifestyle Modifications
Making certain lifestyle modifications can also help manage joint pain and inflammation in psoriatic arthritis. This may include maintaining a healthy weight to reduce stress on the joints, practicing stress management techniques to minimize flare-ups, and avoiding activities that may worsen symptoms. Additionally, a balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and omega-3 fatty acids, may also be beneficial.
- Overall, there are various options for managing joint pain and inflammation in psoriatic arthritis. It is important to work closely with a healthcare provider to find the most suitable approach for your specific condition.
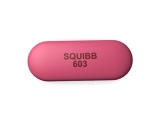
What is Prednisone?
Prednisone is a synthetic corticosteroid medication that is commonly used to treat various inflammatory conditions, including psoriatic arthritis. It belongs to a class of drugs called glucocorticoids, which are derived from the natural hormone cortisol produced by the adrenal glands.
Prednisone works by suppressing the immune system and reducing inflammation in the body. It does this by inhibiting the production of certain chemicals that contribute to the inflammatory response. This helps to alleviate symptoms such as joint pain, swelling, and stiffness associated with psoriatic arthritis.
When prescribed for psoriatic arthritis, prednisone is generally taken orally in tablet form. The dosage and duration of treatment can vary depending on the severity of symptoms and individual response to the medication.
It is important to note that prednisone is a potent medication that can have significant side effects. These can include weight gain, increased appetite, high blood pressure, mood changes, muscle weakness, easy bruising, and increased susceptibility to infections.
Prednisone should be used cautiously and under the guidance of a healthcare professional. The dosages should be carefully monitored and adjusted to minimize side effects while still effectively managing the symptoms of psoriatic arthritis.
How This Steroid Medication Works
Prednisone is a type of medication known as a corticosteroid. It is commonly prescribed to treat various conditions, including psoriatic arthritis. The medication works by suppressing the immune system and reducing inflammation in the body.
Prednisone mimics the effects of a natural hormone produced by the adrenal glands called cortisol. Cortisol helps regulate inflammation and plays a role in the immune response. By taking prednisone, the body's immune system response is dampened, leading to a reduction in inflammation and pain.
When taken orally, prednisone is absorbed into the bloodstream and distributed throughout the body. It binds to receptors on cells, allowing it to exert its anti-inflammatory effects. The medication can also enter cells and influence gene expression, further modulating the immune response.
Prednisone is often used as a short-term treatment option for psoriatic arthritis flare-ups. Its fast-acting nature can help alleviate symptoms quickly, providing relief for patients experiencing joint pain, swelling, and stiffness.
However, it's important to note that prednisone is not a long-term solution for psoriatic arthritis. Prolonged use can lead to a range of side effects, including weight gain, mood changes, increased risk of infections, and osteoporosis. It is typically prescribed at the lowest effective dose and for the shortest possible duration to minimize these risks.
Before starting prednisone or any other medication, it's crucial to consult with a healthcare professional who can assess your specific condition and provide personalized recommendations. They can help determine if prednisone is appropriate for your situation and discuss the potential benefits and risks associated with its use.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Psoriatic arthritis and prednisone"