Surgery while on prednisone
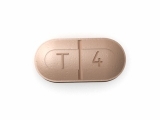
When considering surgery for patients on prednisone, there are several important factors that need to be taken into account. Prednisone is a corticosteroid medication that is commonly used to treat a variety of inflammatory conditions, such as rheumatoid arthritis, asthma, and inflammatory bowel disease. While it can be a highly effective treatment option, it also has the potential to cause complications during surgery.
One key consideration is the impact of prednisone on the immune system. Prednisone works by suppressing the immune system, which can increase the patient's risk of developing infections. This is particularly important in the context of surgery, as the procedure itself can introduce a risk of infection. Surgeons may need to take additional precautions, such as prophylactic antibiotics, to reduce the risk of infection in these patients.
Another important consideration is the effect of prednisone on wound healing. Prednisone can impair the body's ability to heal wounds, which can lead to delayed healing and an increased risk of complications, such as wound dehiscence or infection. Surgeons may need to closely monitor the healing process and may need to adjust the post-operative care plan accordingly, including the use of specialized wound dressings and close follow-up appointments to ensure proper healing.
Additionally, prednisone can have an impact on the body's response to stress. Surgeries are inherently stressful events for the body, and prednisone may further exacerbate this stress response. Patients on prednisone may require additional monitoring and management of their blood pressure, blood sugar levels, and electrolyte balance to ensure their body can adequately respond to the stresses of surgery.
In conclusion, when considering surgery for patients on prednisone, there are several important factors to consider. These include the impact of prednisone on the immune system, wound healing, and the body's response to stress. Surgeons and healthcare providers need to carefully assess these factors and develop a comprehensive plan to minimize the potential risks and complications associated with surgery in these patients.
Prednisone and Surgical Outcomes
Impact of Prednisone on Surgical Outcomes
Prednisone, a corticosteroid medication commonly prescribed for various medical conditions, can have a significant impact on surgical outcomes. It is important for both patients and healthcare providers to be aware of the potential risks and complications associated with prednisone use in the perioperative period.
Infection Risk
One of the main concerns when performing surgery on patients taking prednisone is the increased risk of infection. Prednisone suppresses the immune system, making the patient more susceptible to infections. This can delay wound healing and increase the risk of post-operative complications, such as surgical site infections.
Complications with Wound Healing
Prednisone can also impair the body's natural healing process. It reduces the production of collagen, a protein essential for wound healing, and can cause thinning of the skin. This can lead to poor wound healing, increased scarring, and a higher risk of wound dehiscence (the reopening of a previously closed wound).
Adrenal Insufficiency
Another concern with prednisone use in the perioperative period is the potential for adrenal insufficiency. Prolonged use of prednisone can suppress the body's natural production of cortisol, a hormone produced by the adrenal glands. If the patient abruptly stops taking prednisone before surgery, it can lead to adrenal crisis, a life-threatening condition characterized by low blood pressure and electrolyte imbalances.
Preoperative Preparation
To minimize the risks associated with prednisone use, it is crucial for patients to communicate with their healthcare providers and provide a detailed history of medication use. In some cases, the dosage of prednisone may need to be adjusted prior to surgery to reduce the risk of complications. Adrenal function should also be assessed to ensure proper management during the perioperative period.
Overall, prednisone use can have significant implications for surgical outcomes. Patients and healthcare providers need to work together to optimize patient care and minimize the potential risks associated with prednisone use in the perioperative period.
Risks and Complications
Infection
One of the risks associated with surgery for patients on prednisone is an increased susceptibility to infection. Prednisone is an immunosuppressant medication, which means it can weaken the immune system and make it more difficult for the body to fight off infections. Patients taking prednisone may be more prone to developing surgical site infections or other types of infections after surgery. It is important for surgeons to take extra precautions to prevent infection, such as administering antibiotics before and after the procedure, as well as maintaining a sterile surgical environment.
Poor Wound Healing
Prednisone can also interfere with the body's ability to heal wounds properly. It suppresses the inflammation response, which is essential for initiating the healing process. As a result, patients on prednisone may experience delayed wound healing or other complications related to the surgical incision. Surgeons should closely monitor the healing progress of patients on prednisone and provide appropriate wound care to minimize the risk of complications.
Adrenal Insufficiency
Prednisone is a corticosteroid medication that mimics the effects of cortisol, a hormone produced by the adrenal glands. Prolonged use of prednisone can suppress the adrenal glands, leading to adrenal insufficiency. This condition can cause symptoms such as fatigue, weakness, low blood pressure, and electrolyte imbalances. In the perioperative period, patients on prednisone may require stress-dose steroids to prevent adrenal crisis, a potentially life-threatening condition. Surgeons should consult with the patient's endocrinologist or primary care physician to determine the appropriate steroid management plan prior to surgery.
Increased Risk of Bleeding
Prednisone can thin the blood and increase the risk of bleeding during surgery. This is particularly concerning for procedures that involve significant blood loss, such as major surgeries or operations in highly vascular areas. Surgeons should carefully assess the patient's bleeding risk and consider measures to minimize bleeding during surgery, such as preoperative blood tests, adjusting the dosage of prednisone if possible, and using hemostatic agents or techniques.
Delayed Recovery
Due to the effects of prednisone on the body, patients on this medication may experience a slower recovery from surgery. They may have prolonged pain, limited mobility, or difficulty regaining their pre-operative level of function. Surgeons should set realistic expectations with patients on prednisone and provide appropriate post-operative care, including physical therapy and pain management, to optimize their recovery.
Overall, patients on prednisone undergoing surgery face unique risks and complications. It is crucial for surgeons to be aware of these factors and take appropriate measures to mitigate the potential adverse effects associated with prednisone use.
Preoperative Management
Prior to surgery, it is important to assess the patient's overall health status and evaluate the risks associated with surgery while they are on prednisone treatment. The patient should undergo a thorough medical history evaluation, including a review of their current medications, surgical history, and any underlying medical conditions.
Medication adjustment: Depending on the duration and dosage of prednisone treatment, the patient's medications may need to be adjusted before surgery. Prednisone can suppress the immune system, increase the risk of infection, and delay wound healing. Therefore, it may be necessary to taper the dose of prednisone or switch to an alternative corticosteroid with a shorter half-life.
Infection control: Patients on prednisone are at an increased risk of developing infections. Therefore, preoperative measures to minimize the risk of infection should be implemented. This may include screening for underlying infections, optimizing the patient's immune function through preoperative antibiotics or immunomodulatory therapy, and providing education on proper wound care and infection prevention.
Blood glucose control: Prednisone can cause elevated blood glucose levels, which can impact wound healing and increase the risk of surgical complications. Therefore, it is important to monitor and control blood glucose levels in patients on prednisone. This may involve adjusting the patient's diabetic medications, instituting a restricted diet, or closely monitoring blood glucose levels during the perioperative period.
Adrenal insufficiency: Long-term prednisone use can suppress the adrenal glands' ability to produce cortisol, leading to adrenal insufficiency. In cases where the patient is at risk of adrenal crisis, stress-dose steroids may be necessary perioperatively to ensure adequate adrenal function during surgery.
Cardiovascular considerations: Prednisone can increase blood pressure and fluid retention, which may impact cardiovascular health. Preoperative evaluation should include an assessment of the patient's cardiovascular status, with a focus on managing any preexisting hypertension or heart failure. It may be necessary to optimize blood pressure control with medication adjustments or diuretic therapy to minimize the risk of perioperative cardiovascular complications.
Anesthesia Considerations
When a patient on prednisone requires surgery, there are several considerations that need to be taken into account regarding anesthesia. Prednisone is a corticosteroid medication that can suppress the body's immune response and increase the risk of infections and delayed wound healing. Therefore, it is important for the anesthesiologist to evaluate the patient's overall health and determine if any adjustments need to be made to the anesthesia plan.
Risk of infection: Patients on prednisone may have a higher risk of developing infections due to the immunosuppressive effects of the medication. The anesthesiologist should take proper precautions to minimize the risk of infection during surgery, such as using sterile techniques and maintaining a clean surgical environment. Additionally, prophylactic antibiotics may be considered to further reduce the risk.
Delayed wound healing: Prednisone can impair the body's ability to heal wounds, which can increase the risk of complications after surgery. The anesthesiologist should collaborate with the surgical team to ensure appropriate wound care measures are taken, such as using specialized dressings or providing additional post-operative instructions to promote healing.
Adrenal insufficiency: Long-term use of prednisone can suppress the function of the adrenal glands, which produce natural cortisol. This can lead to adrenal insufficiency, a condition where the body is unable to produce enough cortisol to respond to stress. During surgery, the anesthesiologist should be aware of the patient's adrenal function and consider supplementing with stress-dose steroids to prevent adrenal crisis.
Increased risk of bleeding: Prednisone can thin the blood and impair platelet function, increasing the risk of bleeding during and after surgery. The anesthesiologist should closely monitor the patient's blood clotting parameters and consider appropriate interventions, such as administering antifibrinolytic medications or adjusting the dosage of anticoagulant medications.
Interaction with anesthetic agents: Prednisone can interact with certain anesthetic agents, leading to altered metabolism and potential side effects. The anesthesiologist should review the patient's medication history and consider any drug interactions when selecting and administering anesthesia.
Overall, anesthesia considerations for patients on prednisone involve addressing the increased risk of infection, delayed wound healing, adrenal insufficiency, bleeding, and potential drug interactions. By carefully managing these considerations, the anesthesiologist can help ensure a safe and successful surgical outcome for the patient.
Postoperative Care
After surgery, special care needs to be taken for patients who are currently on prednisone. Here are some key considerations for postoperative care:
Monitoring Medication Dosage
It is important to closely monitor the dosage of prednisone after surgery. The medication may need to be adjusted to ensure optimal recovery and minimize the risk of complications. The healthcare team will work closely with the patient to determine the appropriate dosage based on the individual's condition and surgical outcome.
Monitoring for Infection
Patients on prednisone are at an increased risk of developing infections due to the medication's effect on the immune system. Postoperative care should involve periodic monitoring for signs of infection, such as fever, redness, swelling, or discharge at the surgical site. If any signs of infection are observed, appropriate antibiotics or other interventions should be promptly administered.
Managing Pain and Discomfort
Prednisone can affect the body's response to pain, so it is important to closely monitor pain levels and provide adequate pain management. This may involve a combination of medications and non-pharmacological interventions, such as relaxation techniques or physical therapy. Regular assessment of pain levels and adjustment of pain management strategies are essential for a comfortable recovery.
Addressing Wound Healing
Wound healing may be slower in patients on prednisone due to the medication's impact on collagen production and immune function. Postoperative care should include regular assessment of the surgical incision and any other wounds, along with appropriate wound care. This may involve keeping the incision clean, applying dressings, and ensuring proper nutrition to support healing.
Disease-Specific Considerations
Patients on prednisone often have underlying conditions for which they are taking the medication. The postoperative care plan should take these conditions into account and address any additional concerns or considerations. For example, patients with rheumatoid arthritis may require special joint protection measures, while those with Crohn's disease may need modification of their diet to prevent flare-ups.
Overall, postoperative care for patients on prednisone should be individualized and tailored to address the specific needs and risks associated with the medication. Close collaboration between the healthcare team, the patient, and their caregivers is crucial to ensure a successful recovery and minimize any potential complications.
Long-term Effects and Follow-up
Monitoring and management
Patients on long-term prednisone therapy should receive regular monitoring and management to assess the potential long-term effects of the medication. This may include blood tests to monitor for conditions such as diabetes, osteoporosis, or adrenal insufficiency, which can be side effects of long-term prednisone use.
Patients should also be regularly assessed for signs of Cushing's syndrome, a condition characterized by weight gain, moon face, and buffalo hump. This can occur as a result of prolonged high doses of prednisone and may require dosage adjustments or other interventions.
Follow-up care
It is important for patients on long-term prednisone therapy to have regular follow-up care with their healthcare provider. This allows for ongoing monitoring and adjustment of the medication regimen, as well as addressing any concerns or side effects that may arise.
During follow-up visits, healthcare providers can also discuss strategies for minimizing the long-term effects of prednisone, such as lifestyle modifications or alternative medication options. They can also provide education and support to help patients manage their condition and adhere to their treatment plan.
Psychological considerations
Long-term prednisone therapy can have psychological effects on patients, such as mood changes, irritability, and anxiety. Healthcare providers should be aware of these potential effects and provide support and resources as needed.
Referral to mental health professionals may be beneficial for patients who are experiencing significant psychological distress. These professionals can help patients develop coping strategies, provide counseling, and address any underlying mental health conditions that may be contributing to their symptoms.
Ongoing communication
Ongoing communication between patients and their healthcare providers is essential for long-term prednisone therapy. This allows for the timely identification and management of any complications or concerns that may arise.
Patients should be encouraged to keep a record of any changes or symptoms they experience and to communicate these to their healthcare provider during follow-up visits or through other means. This can help guide treatment decisions and ensure that patients are receiving the most appropriate care.
- Blood tests may be required to monitor for potential side effects of prednisone
- Regular follow-up care is important for ongoing monitoring and adjustment of medication
- Psychological effects of prednisone should be addressed and support provided as needed
- Ongoing communication between patients and healthcare providers is essential
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Surgery while on prednisone"