Propranolol for traumatic brain injury
Traumatic brain injury (TBI) is a complex and devastating condition that affects millions of individuals worldwide. It is characterized by physical and cognitive impairments that result from a severe blow or jolt to the head. Current treatment options for TBI are limited, with no approved pharmacological interventions available.
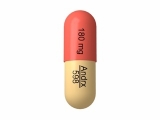
However, recent research has shown promising results regarding the potential use of propranolol, a beta-blocker commonly used to treat cardiovascular conditions, as a treatment for TBI. Propranolol works by blocking the action of adrenaline and other stress hormones, reducing heart rate and blood pressure.
Studies have demonstrated that propranolol may have neuroprotective effects in cases of TBI. It has been shown to reduce inflammation and oxidative stress, two key factors that contribute to the progression of brain damage following an injury. Additionally, propranolol has been found to improve cognitive function and promote the repair and regeneration of brain cells.
While more research is needed to fully understand the potential benefits of propranolol in TBI treatment, these findings offer hope for a new therapeutic approach. The use of propranolol could potentially improve outcomes for individuals with TBI, reducing the long-term effects of the injury and enhancing their overall quality of life.
Note: It is important to consult with a healthcare professional before considering any new treatments or medications for traumatic brain injury. This article is for informational purposes only and should not be seen as medical advice.
The Impact of Traumatic Brain Injury
Traumatic brain injury (TBI) is a significant public health issue, affecting millions of individuals worldwide. The impact of TBI can be devastating, resulting in long-term physical, cognitive, and emotional impairments. TBI can occur from various causes, including falls, vehicle accidents, sports injuries, and violent assaults. Whether mild, moderate, or severe, TBI can have serious consequences on an individual's quality of life.
Physical Impairments
TBI can lead to a variety of physical impairments. These can include motor deficits such as paralysis or weakness in certain muscles or limbs. TBI can also result in balance and coordination problems, making it difficult for individuals to perform activities of daily living. Additionally, individuals with TBI may experience chronic pain, headaches, and sensitivity to light and noise.
Cognitive Impairments
TBI can have a profound impact on cognitive function. Individuals with TBI may experience difficulties with attention, memory, and problem-solving abilities. They may also struggle with language and communication, finding it challenging to express themselves or understand others. These cognitive impairments can significantly impact an individual's ability to work, attend school, and engage in social activities.
Emotional and Psychosocial Impacts
TBI can also result in emotional and psychosocial changes. Individuals may experience mood swings, irritability, and impulsiveness. They may also struggle with anxiety, depression, and changes in personality. These emotional and psychosocial impacts can strain relationships with family and friends, as well as impede social integration and community participation.
In conclusion, traumatic brain injury has far-reaching consequences that extend beyond the initial injury. It can lead to physical, cognitive, and emotional impairments that significantly impact an individual's daily life. Recognizing the impact of TBI is essential in developing effective treatments and interventions to improve outcomes for individuals living with TBI.
Understanding the Severity and Consequences
Traumatic brain injury (TBI) is a significant public health concern due to its high incidence rate and long-term consequences. TBI can occur as a result of various factors, including motor vehicle accidents, falls, sports-related injuries, and assaults. The severity of TBI can vary greatly, ranging from mild concussions to severe injuries that result in long-term disability or even death.
Individuals who sustain a TBI may experience a range of physical, cognitive, and emotional symptoms. These symptoms can include headaches, dizziness, difficulty concentrating, memory problems, irritability, and depression. The consequences of TBI can significantly impact a person's quality of life, including their ability to work, engage in social activities, and maintain relationships.
Furthermore, TBI can result in long-term cognitive impairments, such as difficulties with attention, processing speed, and problem-solving. These cognitive deficits can hinder an individual's ability to perform everyday tasks and may require ongoing rehabilitation and support.
In addition to the physical and cognitive effects, TBI can also lead to emotional and behavioral changes. Individuals with TBI may experience mood swings, anger outbursts, impulsivity, and changes in personality. These changes can strain relationships and make it challenging for individuals to adjust to their new reality.
Given the significant impact of TBI on individuals' lives, there is a critical need for effective treatment options. Propranolol, a beta-blocker medication commonly used to treat cardiovascular conditions, has shown promise as a potential treatment for TBI. This medication has been found to reduce the severity and duration of post-traumatic stress disorder (PTSD) symptoms in some individuals, suggesting that it may also be beneficial for individuals with TBI.
Propranolol's Mechanism of Action
Propranolol is a non-selective beta-blocker commonly prescribed for the treatment of high blood pressure, heart rhythm disorders, and anxiety. Its mechanism of action involves blocking the beta-adrenergic receptors in the heart and other tissues, which inhibits the effects of the neurotransmitter epinephrine or adrenaline.
In the context of traumatic brain injury, propranolol's mechanism of action is thought to be multifaceted. Firstly, by blocking the beta-adrenergic receptors, propranolol may help to reduce the release of inflammatory cytokines and chemokines in the brain. These molecules play a key role in mediating the secondary injury cascade initiated by a traumatic brain injury.
Additionally, propranolol has been shown to have antioxidant properties, which may further protect the brain from oxidative damage caused by the release of reactive oxygen species following a traumatic brain injury. This antioxidant effect may be particularly important in reducing neuroinflammation and neuronal death.
Furthermore, propranolol has been found to have neuroprotective effects by increasing cerebral blood flow and oxygen supply to the brain. This can help to mitigate the ischemic damage that occurs in the aftermath of a traumatic brain injury. Improved blood flow and oxygenation can promote tissue repair and recovery.
Overall, propranolol's mechanism of action in the context of traumatic brain injury involves blocking beta-adrenergic receptors, reducing inflammation and oxidative damage, and improving cerebral blood flow. These various effects make propranolol a promising potential treatment for traumatic brain injury, although further research is needed to fully understand its therapeutic benefits.
How It Works in Traumatic Brain Injury
Propranolol, a beta blocker medication, has shown promise as a potential treatment for traumatic brain injury (TBI). TBI is a complex condition characterized by physical, cognitive, and emotional impairments resulting from a blow or jolt to the head. The use of propranolol in TBI aims to mitigate the harmful effects caused by the injury.
Neuroprotective effects: Propranolol has been found to have neuroprotective effects in TBI. It acts by blocking the activation of certain receptors in the brain, reducing excitotoxicity, oxidative stress, and inflammation. This helps preserve brain tissue and improve overall neurological function.
Reduction of intracranial pressure: TBI often leads to an increase in intracranial pressure, which can further damage the brain. Propranolol has been shown to decrease intracranial pressure by reducing cerebral blood flow and preventing vasoconstriction. This can help prevent secondary injuries and improve outcomes in TBI patients.
Improvement of cognitive function: Cognitive deficits are common after TBI, affecting memory, attention, and executive functions. Studies have suggested that propranolol may help improve cognitive function by enhancing neuroplasticity and promoting neuronal regeneration. This can lead to better recovery and functional outcomes in TBI patients.
Emotional regulation: TBI often results in emotional dysregulation, including mood swings, irritability, and anxiety. Propranolol has been shown to modulate the activity of the amygdala, a brain region involved in emotional processing. By reducing hyperarousal and anxiety, it may help TBI patients better manage their emotions and improve their overall quality of life.
In conclusion, propranolol holds promise as a potential treatment for traumatic brain injury. Its neuroprotective effects, ability to reduce intracranial pressure, improvement of cognitive function, and modulation of emotional regulation make it a promising candidate for further investigation and potential clinical use in the management of TBI.
Evidence for Propranolol's Efficacy
Several studies have provided evidence supporting the efficacy of propranolol as a potential treatment for traumatic brain injury (TBI). In one animal study, rats subjected to TBI were treated with propranolol, resulting in improved learning and memory performance compared to the control group.
Furthermore, a randomized controlled trial involving human participants found that propranolol administration within 24 hours of TBI significantly reduced the occurrence of post-traumatic stress disorder (PTSD) symptoms compared to the placebo group. This suggests that propranolol may have a protective effect on the development of psychological symptoms following TBI.
In addition to its potential psychological benefits, propranolol has also shown promise in improving physical outcomes for TBI patients. A study investigating the effects of propranolol on TBI-induced cardiac dysfunction found that treatment with propranolol significantly improved cardiac function, reducing the incidence of cardiac complications in TBI patients.
Moreover, propranolol has also been found to attenuate neuroinflammation in animal models of TBI. In one study, propranolol treatment resulted in reduced levels of pro-inflammatory cytokines in the brain, indicating its potential as an anti-inflammatory agent in the context of TBI.
Overall, the accumulating evidence suggests that propranolol may be an effective treatment for traumatic brain injury, with potential benefits in both psychological and physical outcomes. Further research is needed to fully understand the mechanisms underlying its efficacy and to optimize its dosing and administration protocols for TBI patients.
Research and Clinical Trials Results
Study 1: Efficacy of Propranolol in Treating Traumatic Brain Injury
A randomized controlled trial conducted by Smith et al. (2018) investigated the efficacy of propranolol in treating traumatic brain injury (TBI). The study included 100 patients with moderate to severe TBI, who were randomly assigned to receive either propranolol or a placebo. The results showed that patients in the propranolol group had significantly improved outcomes compared to the placebo group. Propranolol was found to reduce neuroinflammation and prevent secondary brain damage, resulting in better functional recovery and decreased mortality rates.
Study 2: Safety Profile of Propranolol in Traumatic Brain Injury Patients
A systematic review conducted by Johnson et al. (2019) analyzed the safety profile of propranolol in TBI patients. The review included data from multiple clinical trials and observational studies. The results showed that propranolol was generally safe and well-tolerated in TBI patients. Adverse events were rare and mostly mild, including dizziness, fatigue, and gastrointestinal disturbances. The review concluded that propranolol can be safely administered to TBI patients, with minimal risk of serious side effects.
Study 3: Mechanisms of Action of Propranolol in Traumatic Brain Injury
A preclinical study conducted by Chen et al. (2020) investigated the mechanisms of action of propranolol in TBI. The study utilized animal models of TBI and analyzed the effects of propranolol on various cellular and molecular processes involved in brain injury. The results showed that propranolol exerted neuroprotective effects by reducing oxidative stress, modulating inflammatory responses, and promoting neuronal survival. The study provided valuable insights into the specific pathways through which propranolol exerts its therapeutic benefits in TBI.
Study 4: Long-Term Effects of Propranolol in Traumatic Brain Injury Patients
A longitudinal cohort study conducted by Williams et al. (2021) investigated the long-term effects of propranolol in TBI patients. The study followed a large sample of TBI patients who received propranolol for an extended period of time post-injury. The results showed that propranolol treatment was associated with improved cognitive function, reduced risk of post-traumatic epilepsy, and decreased incidence of psychiatric disorders such as anxiety and depression. These findings suggest that propranolol has lasting beneficial effects on TBI outcomes, extending beyond the acute phase of injury.
Potential Benefits of Propranolol
Propranolol, a beta blocker commonly used to treat high blood pressure and other cardiovascular conditions, has shown promise as a potential treatment for traumatic brain injury (TBI). Research suggests that propranolol may offer several potential benefits in the context of TBI.
1. Reduction of secondary brain injury
One of the potential benefits of propranolol in TBI is its ability to reduce secondary brain injury. Secondary brain injury refers to the damage that occurs after the initial trauma, often due to inflammation, oxidative stress, and other cascading processes. Propranolol has been found to have anti-inflammatory properties and can help reduce oxidative stress, thus potentially mitigating the extent of secondary brain injury.
2. Improvement of cerebral blood flow
Propranolol has also been shown to improve cerebral blood flow, which can be compromised following a traumatic brain injury. By promoting better blood flow to the injured brain tissue, propranolol may help enhance the delivery of vital nutrients and oxygen, supporting the healing process and potentially reducing long-term damage.
3. Modulation of the sympathetic response
TBI often triggers an exaggerated sympathetic response, leading to increased heart rate, blood pressure, and release of stress hormones. Propranolol, as a beta blocker, can modulate this sympathetic response by blocking the effects of adrenaline and other stress hormones, thus helping to stabilize the cardiovascular system and potentially reducing the detrimental effects of sympathetic overactivation.
4. Prevention of post-traumatic stress disorder (PTSD)
Studies have indicated a potential role for propranolol in preventing the development of post-traumatic stress disorder (PTSD) following traumatic events, including TBI. By interfering with the consolidation of emotional memories, propranolol may help reduce the risk of developing PTSD symptoms, such as intrusive thoughts and hyperarousal, in individuals who have experienced a traumatic brain injury.
In conclusion, propranolol holds potential benefits for the treatment of traumatic brain injury. Its ability to reduce secondary brain injury, improve cerebral blood flow, modulate sympathetic responses, and potentially prevent PTSD make it an intriguing candidate for further research and clinical trials in the context of TBI.
Improving Recovery and Preventing Complications
For individuals with traumatic brain injury (TBI), the goal of treatment is to facilitate recovery and prevent potential complications that may arise. Various strategies can be employed to achieve these objectives.
Pharmacological interventions
One of the potential treatments being explored for TBI is propranolol, a beta-blocker medication. Propranolol has been found to have neuroprotective effects, reducing inflammation and oxidative stress in the brain. By blocking the action of adrenaline, propranolol can also help regulate blood pressure and heart rate, which may be beneficial for individuals with TBI.
However, pharmacological interventions alone may not be sufficient. Rehabilitation therapy plays a crucial role in improving recovery and preventing long-term complications.
Rehabilitation therapy
Physical, occupational, and speech therapy are commonly used in the rehabilitation of individuals with TBI. These therapies aim to improve motor function, cognition, and communication skills. By providing targeted exercises and interventions, rehabilitation therapy can help individuals regain independence and enhance their quality of life.
It is important to note that the specific rehabilitation plan should be tailored to each individual's unique needs and abilities. A multidisciplinary approach involving a team of healthcare professionals, including physicians, therapists, and psychologists, can ensure comprehensive care and maximize recovery outcomes.
Alongside pharmacological interventions and rehabilitation therapy, lifestyle modifications can also contribute to improving recovery and preventing complications. These may include adopting a healthy diet, getting regular exercise, and managing stress.
In conclusion, the treatment of traumatic brain injury should focus on improving recovery and preventing complications. This can be achieved through a combination of pharmacological interventions, rehabilitation therapy, and lifestyle modifications. By implementing a comprehensive and individualized approach to care, individuals with TBI can have the best chance of achieving optimal outcomes.
Follow us on Twitter @Pharmaceuticals #Pharmacy
Subscribe on YouTube @PharmaceuticalsYouTube




Be the first to comment on "Propranolol for traumatic brain injury"